back (05.16.2004/04.16.2006)
 DrTim homepage link
DrTim homepage link
Obstetric Anesthesia for OBGYNS
Timothy Bilash MD, OBGYN
May 16, 2004
www.DrTimDelivers.com
Index
- References
- Other Articles
- Key to abbreviations
- Hemodynamics
- Afferent (Sensory) Visceral System [G&G p56-57]
- Efferent (Motor/Gland) Systems
- Sympathetic Drugs [G&Gp144]
- Pain Drugs
- PREGNANCY
- Conduction blockade [NORp334]
- Maternal Complications of Regional Anesthesia
- Fetal status
- Thermoregulation and anesthesia
- Anesthesia Services
- References
-
[BAR] BarashP et al,
Handbook of Clinical Anesthesia 4th Ed 2001
-
[BSOG] Tim Chard et al,
Basic Sciences for Obstetrics and Gynecology
-
[COL] Pietro Colonna-Romano, MD et al,
Epinephrine-Induced Tachycardia is different from Contraction Associated Tachycardia in Laboring Patients
Anesth Analg 1996;82:294-6]
-
[DAV] Davison, J. Kenneth et al, editor (RECOMMENDED)
Spinal, epidural and caudal anesthesia
Clinical Anesthesia Procedures of the Massachussetts General Hospital 4th ed
-
[ENG] Engberg G, Wiklund L,
The circulatory effects of intravenously administered ephedrine during epidural blockade,
Acta Anaesthesiol Scand Suppl 1978;66(66):27-36
-
[EST] Easterling TR, Obstet Gynec 78:348.1991 Hemodynamics
-
[FIN] Finucane BT,
Complications of Regional Anesthesia, 1999
-
[G&G] Goodman and Gilman
-
[HOY] An anestehsiologist talks analgesia choices
Anna Nidecker, OBGYN News Nov1, 1996, p21
Dr. Callum R. Hoyt, chief of obstetric anesthesiology at Case Western Reserve, at a meeting on obstetrics and obstetric anesthesia by St. John Hospital and Medical Center in Detroit
-
[HUR] Alexander, RW, Hurst's the Heart
-
[KAU] Kaufman, Horacio
Cardiology Clinics 15(2)1997:182
-
[KAU2] Kaufman, horacio MD
neurologists viewpoint (syncope)
cardiology clinics 15(2); may1997:177-194
-
[KIN] Kinsella SM, Black AM
Reporting of 'hypotension' after epidural analgesia during labour. Effect of choice of arm and timing of baseline readings.
Anaesthesia 1998 Feb;53(2):131-5
-
[LEI] Leighton BL, Halpern SH, Wilson DB, Anesthesiology Lumbar sympathetic blocks speed early and second stage induced labor in nulliparous women, 1999 Apr;90(4):1039-46
Published erratum appears in Anesthesiology 1999 Aug;91(2):602
-
[MOB] Manual of Obstetrics 4th Ed, Evans A and Niswander K
-
[MIL] Miller, Ronald D., Anesthesia 5th ed
-
[MOR] Morgan P
The role of vasopressors in the management of hypotension induced by spinal and epidural anaesthesia,
Can J Anaesth 1994 May;41(5 Pt 1):404-13
Department of Anaesthetics, University Hospital of Wales, Heath Park, Cardiff, South Glamorgan, United Kingdom.
-
[MUE] Mueller, Michael David, MD et al
Higher Rate of Fetal Acidemia after Regional Anesthesia than for Elective Cesarian Delivery
Obstet and Gynecology, july1997, 90(1):131-34
-
[NOR] Norris, Mark C,
Obstetric Anesthesia 1999
-
[OMO] Omoigni, Sota
Anesthesia Drugs Handbook 3rd ed
(blackwell science)
-
[PAL] Palmer CM, D’Angelo RD, Paech MJ
Handbook of Obstetric Anesthesia 2002
-
[PDR] Physicians Desk Reference
-
[SAE] Yuka Saeki PhD et al,
The effects of Sevoflurane, Enflurane, and Isoflurane on Baroreceptor-Sympathetic reflex in Rabbits,
Anesth Analg 1996;82:342-8
-
[SES] Sessler DI
Perioperative Heat Balance
Anestheliology 2000;92:578-96
-
[THO] Thorp, James A, MD
Clin Obs Gynecol 1999(42:4);785-801
Epidural Analgesia during labor
-
[WIL] Pritchard, Williams Obstetrics 20th ed
-
[VER] Vercauten MP, et al,
Prevention of Hypotension by a single 5-mg dose of ephedrine during small-dose spinal anesthesia in prehydrated cesarian delivery patients,
Anesth Analg 200 Feb;90(2):324-7
-
[USPDI] United States Pharmacologic Directory
-
Other Articles
- Anesthesiology 1993 Dec;79(6):1250-60
Effects of epidural and systemic lidocaine on sympathetic activity and mesenteric circulation in rabbits.
Hogan QH; Stadnicka A; Stekiel TA; Bosnjak ZJ; Kampine JP
-
Adv Pharmacol 1994;31:471-83
Effects of epidural anesthesia on splanchnic capacitance.
Hogan QH; Stadnicka A; Kampine JP
-
Anaesthesia 1998 Feb;53(2):131-5
Reporting of 'hypotension' after epidural analgesia during labour. Effect of choice of arm and timing of baseline readings.
Kinsella SM, Black AM
-
Anesth Analg 2000 Mar;90(3):632-7
A comparison of epidural analgesia with 0.125% ropivacaine with fentanyl versus 0.125% bupivacaine with fentanyl during labor.
Meister GC, D'Angelo R, Owen M, Nelson KE, Gaver R
-
Cah Anesthesiol 1995;43(6):547-53
Conduction anesthesia and the newborn infant.
Palot M, Visseaux H, Botmans C [Article in French]
-
effects of morphine epidurals on neurobehavioral scores
-
Anesth Analg 1996;82:294-6
Epinephrine-Induced Tachycardia is different from Contraction Associated Tachycardia in Laboring Patients
Pietro Colonna-Romano, MD et al
-
Anesth Analg 2000 Nov;91(5):1310-1
Ropivacaine and bupivacaine with fentanyl for labor epidural anesthesia.
Pinder AJ, Dresner M
-
Eur J Obstet Gynecol Reprod Biol 1995 May;59 Suppl:S17-29
Influence of epidural analgesia on fetal and neonatal well-being.
Scherer R, Holzgreve W
-
neonatal effects of narcotics in epidurals
-
Acta Anaesthesiol Belg 2000;51(2):131-4
Analgesia for labor pain with ropivacaine.
Van de Velde M
-
Anesth Analg 1994 Feb;78(2):293-300
Vincent RD et al
-
Key to abbreviations
-
[A?]
author question
-
[ISLT]
It Seems Likely That
- [ANOTE] Authors Note
- Hemodynamics
- Blood pressure measurement
[MILp1121-1124]
- systolic1st sound (when needle fluctuates marks systolic blood pressure manually)
- diastolic 4th vs 5th sound
- rate of deflation = 2mmHg/heartbeat
improves accuracy
- Mean Arterial Pressure (MAP)
= [systolic BP + 2 x (diastolic BP)] / 3
[WILp1061]
- diastolic contributes 2/3 of the mean value
- Hypotension
is defined as systolic BP < 90-100 mmHg, or a decline of 20-30% from baseline. [VER]
- If recognized and treated propmtly, transient maternal hypotension does not usually cause maternal or neonatal morbidity. [MILp2043]
- Current data indicate that hypotension of 50 to 65 mm Hg (MAP) is safe in healthy (non-pregnant) patients. [MIL p1486]
- automated monitoring [MILp1122]
- peak amplitude
of aortic pulsations corresponds closely to the true mean
arterial pressure (dynamap)
- systolic
and diastolic
pressure values are derived
using proprietary formulas that examine the rate of change of the pressure pulsations
- systolic pressure is chosen when pulsations are at 25 to 55 percent of maximum
- diastolic pressure is more difficult to determine, but commonly placed where pulse amplitude decreased by 80 percent
- [ISLT] mean blood pressure is a better measure for epidural with automated pressure measurement
- effect of tachcardia on accuracy [?]
- measurement on distal digital arteries can provide continuous values [MILp1123]
- Blood pressure measurement issues
[MILp1123, KIN]
- where to measure BP
- for lower central vessel blood pressure measurement in the lateral position, the blood pressure cuff should be placed on the dependent arm (with or without epidural)
- similar
to blood pressure in either arm in the semirecumbent
position
- higher than in the upper arm an average of 10 (systolic) and 14 (diastolic) mmHg
- the arterial pressure waveform changes its morphology as it is transmitted to the vascular tree.
- systolic pressure progressively increases moving to the periphery
from the central aorta
- peripheral systolic overestimates central systolic
- larger arteries of the upper arm and thigh have equal systolic pressures
- [ISLT] less flow at higher pressure peripherally in each smaller vessel
- pulse pressure is wider from a peripheral artery
then from a more central location. [MILp1131]
- pulse pressure increases with stroke volume
or ejection velocity
- pulse pressure increases as peripheral resistance (TPR) decreases
[HUR p257]
- mean
femoral, brachial, and popliteal pressures are equal [HUR p257]
- large differences between peripheral and central arterial pressures may be seen in patients with shock
. [MIL]
- Femoral artery systolic pressure may exceed radial artery systolic pressure by more than 50 mm Hg in septic patients.
- Anesthetics (particularly neuraxial block) or changes in patient temperature produce pressure gradients that alter central to peripheral arterial pressure measurements. [MILp1130]
- marked disagreement occurs for indirect vs direct pressure measurements [MILp1123]
- indirect measurements vary between patients, over time, and with changing hemodynamic conditions
.
- indirect method
tends to underestimate systolic
pressure, underestimate diastolic pressure when phase 5
is used, overestimate diastolic
pressure by several mmhg when phase 4
is used. [HURp256]
- indirect method phase 4 (muffled sound) underestimates pulse pressure [HURp256]
- indirect method phase 5 (loss of sound) overestimates pulse pressure
- indirect tends to underestimates BP
- immediate reinflation
for multiple pressure determinations result in venous congestion which may falsely decrease the systolic and increase the diastolic
readings.
- ie, decrease in pulse pressure
- shock or vasopressors can attenuate sound generation
- Factors affecting arterial pressures [HURp256]
- peak systolic pressure is greater
during expiration
by as much as 10 mmhg
- [ISLT] inhalation lowers peak systolic BP (lamaze) vs prevents increase (moderates sympathetic increase)
- Pulse Pressure
- stroke volume
and ejection velocity
increase pulse pressure.
- fever, anemia, hot weather, excercise, pregnancy, hyperthyroidism increase pulse pressure
- AV fistula increases
pulse pressure
- lowers diastolic or raises systolic, or both [A?]
- [ANOTE] reduce systolic vs diastolic blood pressure more [A?]
- Lo CO/Hi SVR would increase PP
- Hi CO/Hi SVR would increase MAP and PP
- Lo CO/Lo SVR would decrease MAP and decrease PP
- Hi CO/Lo SVR would decrease PP
- BP increases throughout the day
into early evening.
- sudden drop to lowest during early deep sleep
- does this reset sympathetic/ parasympathetic tone (sleepy when wake from nap) [A?]
- gradual increase in sympathetic tone
- [ISLT] compensates vascular leakiness later in day [A?]
- With increasing age
, the aorta has stiffer walls. [HURp256]
- This results in an increase in systolic arterial pressure
with less change in diastolic pressure.
- [ISLT] arteriosclerosis (hardened vessels) affects systolic BP more[?]
- [ISLT] atherosclerosis (plaques) affects diastolic BP [?]
- duration of systole shortens with age
- increased sympathetic
- Some authorities do not recommend drug treatment of hypertension until BP is > 160/95, and or diastolic blood pressure >95, in the absence of target organ disease or risk factors. [p1673]
- Elderly benefit from treatment when the systolic BP only is elevated >160.
-
Systolic BP
is a more reliable predictor of cardiovascular
events than diastolic
.[HURp1674] ???
- systolic raises 2x more for same increase in mean pressure
- ie, need half the increase in diastolic to see same increase in mean, would make disatolic LESS sensistive
- affects pulse pressure more
- physiologic range of normal may overlap the statistical range of abnormal in any individual
- [ANOTE] hemorrhagic vs thrombotic stroke vs MI, vs mean/diastolic [?]
- [ANOTE] predictive value of mean BP [?]
- [ISLT] mean (diastolic) BP is more predictive of cerebral stroke?
-
Vascular Anatomy
- parts of vascular systems affected and at which level
- peripheral arteries
- peipheral arterioles
- peripheral pre-capillary sphincters
- post capillary sphincters
- splanchnic areteries
- splanchnic veins
- peripheral veins
- Determinants of Cardiac Output
[MIL p636, DAV p273]
-
CO = MAP/SVR
-
Blood Pressure
(MAP)
-
Heart rate
(HR)
-
Myocardial compliance
- Contractility (CT)
- Preload
(
volume
returning to heart)
- preload = VR (venous return) or SV (stroke volume)
- ventricular filling
at the end of diastole (resting)
- venous capacitance vessels
- splanchic (portal vein)
- CVP <-- preload (reflects low pressure of cycle)
- vascular tone
- blood volume
-
Afterload
(
resistance
the heart pumps into)
- arterial resistance
at the beginning of systole, systemic vascular resistance (
SVR
)
- technically ventricular wall tension during systole, so diseased heart affects
- PRE
capillary sphincters vasoconstrict
- controls BP, systolic blood flow
- POST
capillary sphincters, controls pooling
- reflects high pressure of cycle (systolic)
- Intraocular pressure measurement reflects systemic vascular resistance [Diprovan in PDR]
-
Organ blood flow = (MAP-organ venous pressure)/(organ vascular resistance)
- Sympathetic cardiac tone
(SCT)
- Parasympathetic cardiac tone
(PCT)
- Sympathetic mesenteric venous tone
(MVT)
- increases VR and thus CO
- if low less blood returns to heart
- Sympathetic splanchnic capacitance tone
- Systemic Parasympathetic tone
-
Cardio/Neural/Vascular System Blocks
- Neural block categories (global/regional)
- Sensory block
- Motor block
- Sympathetic block
- Parasympathetic block
- CNS block
-
Vascular block
- systemic artery tone (affects pressure, CO)
- SVR (precapillary tone)
- systemic vein tone (affects CO)
- VR (post capillary tone)
- mesenteric vein tone (affects CO)
- splanchinic capacitance tone (VR, CO)
- portal vein tone (CO)
-
Heart block
- rate (chronotropy)
- contractility (inotropy)
- volume (CO)
-
Neural Transmitters
- Afferent Sensory
fiber neurotransmitters [PALp34]
-
Glutamate
(primary sensory afferents)
- Substance P
(primary sensory afferents)
-
Acetyl Choline (AcH
interneurons of dorsal gray matter)
-
Inhibitory Sensory
-
Norepinephrine (NE
descending efferent inhibits ascending afferents)
- Efferent
fiber neurotransmitters
- Cholinergic- the neurotransmitter is acetylcholine (
AcH
) [p58 G&G]
- all preganglionic parasympathetic
fibers (=from CNS to autonomic ganglia
)
- all postganglionic parasympathetic
fibers (
=
from ganglia to organs
)
- a few postganglionic sympathetic
fibers (beta2, sweat glands and vasodilation, from ganglia to organs
)
-
Adrenergic
- the neurotansmitter is norepinephrine (
NE
)
- majority of postganglionic sympathetic
fibers
- postganglionic sympathetic fibers blocked by spinal sympathetic/ epidural block
- Vagus System Efferent
structure [MILp635]
-
RIGHT vagal
and RIGHT stellate ganglion
- innervate right heart, SA node
- more of an effect on heart rate
-
accelerator sympathetic fibers
-
parasympathetic vagus slowing (mechanism unclear, may decrease cAMP)
- LEFT vagal
and LEFT stellate ganglion
- innervate left heart, AV node
- more of an effect on contractility
- sympathetic adrenergic fibers
- alters AV nodal conduction
- duration and intensity of systole (increases mean pressure
)
- [ISLT] one sided or level of block affects one more than other
-
anatomical differences in right and left distributions and pathways, although some overlap
- atria have higher NE levels (greater sympathetic inervation) than ventricles
-
Sensory, Motor and Autonomic distribution of spinal nerves
-
Afferent
autonomic nerves innervate visceral sensations and viscerosomatic reflexes
- at spinal segmental levels
much higher than would be expected from skin dermatomes
[DAVp206]
- efferent affects to motor, adrenal, renal [?]
- sensory inervation corresponding to skin dermatomes for obstetrics [DAVp207]
- lower abdomen and back T11 to L2
-
T10 required for vaginal/uterine anesthesia
- [ISLT model]
- CNS nuclei pre-amplifiers to the brain (incoming)
- Ganglia post-amplifiers to the organs (outgoing)
- Hemodynamic Control
[recommended chapter, DAVp273]
-
Autoregulation
- 75% of all local blood flow is controlled by metabolic substances
- anesthetics inhibit autoregulation, organ perfusion becomes pressure-dependent
- [ANOTE?] any local uterine muscle or blood flow effects from local absorption of anesthetic into uterine veins and lymphatics
- Sympathetic / Adrenergic
[DAV p273]
- systemic outflow receptors, generally non-local
- receptors [DAVp273]
-
alpha
(NE>EPI>ISO)
-
beta
(ISO>EPI>NE)
-
dopa
(Dopamine)
- Alpha1
- increases BP, maintains CO, increases SVR
- excitatory POST
synaptic (receiver side)
- arteriolar and venous constriction
- smooth muscle and glands
[G&G p139]
- vascular, heart, uterus, skin, intestine, splanchnic bed smooth muscle
- relaxation of intestinal tract
-
decreases heart rate, increases contractility
- ephedrine has these effects from NE release
- Alpha2
- maintains BP, decreases CO, increases SVR
[G&G p139,140; BAR p121]
- inhibitory PRE
synaptic alpha2 (CNS, sender side)
- large epicardial vessels
- inhibits NE
release
- decreases sympathetic outflow
leading to hypotension and bradycardia
- possibly inhibits acetylcholine
release [G&Gp139]
-
relaxation of the GI tract smooth muscle [G&G p139]
-
venous return
- excitatory POST
synaptic alpha2 (receiver side)
- small coronary arteries, peripheral venous vessels (no alpha1)
- cerebral cortex, platelets, uterus, parotid gland [G&G p139]
-
vasoconstriction
and hypertensive
alpha2 responses (with alpha1)
- CNS- analgesia
and anesthesia
effects (dorsal horn alpha2) [NOR p404]
- AV shunt to redistribute blood in hypothermia
- Alpha3
- brown fat inervation to produce heat
- Beta1 - cardiac [G&G p139]
- myocardium, SA node, ventricular conduction system, adipose
-
increases cardiac function (BP, HR, CO)
- increases lipolysis
(fatty acid release)
- Beta2 - smooth muscle and glands [DAVp273]
-
inhibitory at smooth muscle (relaxation)
- vascular, bronchial, uterine, skin, smooth muscle
- vasodilation, bronchodilation, uterine relaxation
- gluconeogenesis, insulin release, potasium uptake by cells (glucogenic into cells)
- Dopa1 - renal and mesenteric [DAVp273]
- post
synaptic
- renal and mesenteric vascular smooth muscle
-
vasodilation
- Dopa2 - indirect [DAVp273]
-
pre
synaptic
-
inhibits NE
release
-
Parasympathetic / Cholinergic
- mainly discrete and localized discharge
-
Vaso / Neuroactive Substances
-
Receptors
-
Sympathetic
- alpha sympathetic
- beta sympathetic
- dopaminic
-
Parasympathetic
- AcH
- muscarinic
- nicotinic (striated muscle)
-
Substances
- Angiotensin I
- Angiotensin II (renal)
- Angiotensin III
- ANF
- AVP
- Dopamine
- Endothelin
- Epinephrine (adrenal)
- Estrogen
- Histamine
- NO
- Norepinephrine
- Progestin
- Renin (active)
- Relaxin
- Seratonin
- Vasopression (hypothalamus)
- Intermediaries
-
Thromboxane A2
-
Prostaglandins
-
PGI2
associated with enhanced release of
-
AVP
-
active renin
-
epinephrine
-
thromboxane A2
-
Blood pressure maintenance
-
Vascular Blood pressure regions
-
Heart
- LV
-
Artery
- aorta
- upper (brachial)
- systolic
- diastolic
- lower (femoral)
- systolic
- diastolic
-
Vein
- upper (suprarenal IVC)
- systolic
- diastolic
- lower (infrarenal IVC)
- systolic
- diastolic
- Splanchnic Vein (mesenteric)
-
Central Vein (RA)
-
Cardiovascular parameters
-
Heart Rate (HR, rate)
-
Contractility (BP, pressure)
-
Stroke Volume (SV, volume)
- Cardiac Output (CO, volume rate)
-
Cardiovascular Control Points
- cardiac baroreceptors (carotid sinus, aortic arch)
- cardiac chemoreceptors (carotid and aortic bodies)
- cardiac sympathetic tone (beta1 inotropy)
- cardiac sympathetic tone (beta1 chronotropy)
- humoral sympathetic tone (EPI, NE, Ephedrine, direct active drugs)
- upper arterial tone (alpha1, beta2, NE, EPI)
- lower arterial tone (alpha1, beta2, NE, EPI)
- post capillary tone (alpha2, beta2 EPI, NE)
- venous tone (alpha2, beta2, EPI, NE)
- splanchnic tone (alpha, beta2, NE, EPI)
- renal tone (alpha, beta2, NE, EPI)
- adrenal tone (alpha, beta2, EPI)
- uterine tone (alpha, beta2, NE, EPI)
- vagal sympathetic tone (beta1, NE)
- vagal parasympathetic tone (AcH, negative chronotropy)
- parasympathetic vasodilator tone (NO, AcH)
-
Hypotension modulator mechanisms
- afferent sympathetic peripheral baroreceptor reflex (stimulation or block)
- counters the increase or decrease in systemic vascular resistance (SVR) [MIL]
-
efferent sympathetic cardiac
stimulation or block (cardiac speedup or slowdown)
- upper sympathetic efferent vascular block (decreased venous return)
- lower sympathetic efferent
vascular block (decreased venous return)
- efferent parasympathetic cardiac
vagal stimulation or block (cardiac slowdown or speedup)
- Neurally Mediated Syncope (NMS- Vasovagal)
[KAU p182+]
-
appropriate
increase in:
-
Epinephrine (adrenal)
-
AngiotensinII (renal)
-
Vasopression (hypothalamus)
-
Endothelin release (prostaglandins)
- inappropriate changes:
- NE drops (sympathetic nerve activity SENA and Norepinephrine fail to rise)
- NO synthesis
is activated
- parasympathetic rise in AcH
- possibly beta2-mediated induced by a rise in adrenaline
- 11-OH corticosteroids
(adrenal mineralcortcoid)???
-
hypovolemia
probably factor
- small preload with water abolishes
- autonomic failure causes exaggerated sodium loss and polyuria while supine
- volume depletion and hypotension worse in AM
- increasing salt intake with fludrocortisone improves orthostatic response [p184]
- salt-deficit syndrome in chronic fatigue syndrome
- semi-sitting prevents naturesis and possibly increases renin
- [ISLT] epidural has similar effect
- plasma catecholamines
-
dopamine
- gravity is other vasovagal cause (sudden change in posture)
- bradycardia is not causative, although present
-
Atrial Natriuretic Peptide (ANP)
- causes vasodilation and naturesis
- released with volume loading
- Nitric Oxide (NO) [HURp1637]
- synthesized from L-arginine
through nitric oxide synthetase
- important for vasodilatation
- deficit can be reversed by ACE inhibitors and L-arginine
-
Renin-Angiotensin
- Renin-angiotensin and Vassopressin systems are activated under conditions of hypovolemia [MILp 1475]
- Aldosterone released from adrenals secondary to lower blood sodium and blood volume
-
Renin from the kidney caused by reduced levels of aldosterone, from the adrenals
- Angiotensinogen is converted to Angiotensin I by renin
-
Angiotensin I is cleaved by acetylcholinesterase (ACE in the lungs and local tissues) rapidly to Angiotensin II (a potent vasoconstrictor) [HURp1639]
- Valsalva
[MILp641]
- increased intrathoracic pressure from holding breath and bearing down
- increased CVP (Central Venous Pressure)
- deep breathing reduces CVP
- a mechanism of effects of stress [?]
- decreased venous return to heart
- increases heart rate via baroreceptor reflex sympathetic
stimulation
-
Cerebral auto regulation
[MILp699]
- range of autoregulation is 70 to 150 mm Hg (MAP)
- above and below this range cerebral blood flow is pressure dependent
- cerebral blood flow remains constant until MAP falls to 65 mmHg.
- When MAP fell below this level, the pressure-flow relationship was linear.
- When the MAP falls below 50 mmHg, CBF no longer response to changes in PaCO2 [MILp1481]
- somewhat higher ranges in humans than animals
- [ISLT] hemorrhagic shock (high sympathetic tone) has a lower cerebral blood flow at a given MAP, as compared to sympathetic block by drugs (low sympathetic tone) for same pressure
-
Epidural effects
- motor block
- decreased vascular resistance
- epidurals produce maternal atrial tachycardia vs wide pulse pressure
- chronotropy vs stroke volume increase with underfilling [KAU2 p189]
-
Vascular complications of Anesthesia
- Hypothermia
[SES]
- neurally mediated
- regional anesthesia redistributes heat to the periphery, core gets colder
- patients feel warm
- put sweats on patients with epidural
- upper non-anesthetized parts can shiver, but doesnt do much
- effects AV shunt areas (toes, finders) primarily redistributes blood to periphery
- get redistribution, not total body heat loss
- alpha1 augmented by local alpha2
- reduces shivering (central inhibition, proportional to block height)
-
general anesthesia reduces vasoconstriction (central inhibition)
- overcome as body temperature drops, start to shiver
- Hypotension
[DAVp247]
- significant decrease in BP (thru contractility, SVR, venous return effects)
-
Contractility (CNT)
- vagal reflexes (parasympathetic) and systemic anesthestics (particularly bupivacaine) are cardi-depressant (most anesthetics are cardio-depressants)
- opiates are not cardiac depressants
-
Systemic Vascular Resistence (SVR)
- isoflurane reduces SVR
- bowel manipulation may cause hypotension thru release of vasoactive metabolites
-
Venous return (VR)
- hypovolemia
- caval compression (pregnancy)
- increased venous pooling
- increased splanchnic capacitance from sympathetic blockade
(decreases VR)
-
Sympathetic tone [FINp196]
- arteries retain some intrinsic tone after sympathetic block, veins do not
- vasoactive metabolites can further dilate arteries (organic acids, hypercarbia, endotoxin [?])
-
Bradycardia
decreases Cardiac Output CO (low rate)
-
Tachycardia
decreases Cardiac Output CO (decreased diastolic filling time, stroke volume)
- neuraxial blockade hypotension is the result of decreased SVR
or decreased CO [FINp196-7]
- relative contributions of decreased SVR and CO from case to case are quite variable
- unsure as to which is more important in any given case
- significant reduction in SVR during neuraxial blockade
- vasodilation effects of lower sympathetic blockade
is modified by compensatory increase in sympathetic tone and vasoconstriction in unblocked areas, resulting in little change in total SVR (redistribution).
- higher level sympathetic block
or concomittant general anesthesia
increases the likelihood for hypotension.
- sympathetic blockade usually several segments above sensory block, but is not as easily quantified as the extent of sensory anesthesia
.
-
venodilation decreases venous return, increases capacitance vessel blood volume
-
CO is relatively unchanged during spinal anesthesia unless the drop in systolic blood pressure is greater than 25%.
- heart rate increase compensates for decreased stroke volume, maintaining CO
- below 90mmHg, CO falls significantly
- 80% of surgical
patients have decreased SVR
when hypotensive
-
nonoperative
patients have reduced CO
when hypotensive
- bupivacaine reduces the risk of hypotension ???
- treatment of hypotension
- decrease anesthetic depth
- volume expansion
- reposition in Trendelenberg to increase VR
- correct mechanical obstructions or pressure in cavities
- treat cardiac causes, bradycardia
-
Hypertension
- definition
- systolic >140 (previously also increase of 30 mmHg)
- diastolic >90 (previously also increase 15 mmHg)
- diastolic has twice the effect on MAP as the systolic
- catecholamine excess (inadequate anesthesia)
- systemic absorption of vasoconstrictor ([ISLT] ropivacaine does this too, it is a vasoconstrictor)
- bladder distension
- indigo carmine dye (alpha agonist)
- total body water is normal in hypertension [HURp1637-38]
- Decrease of plasma volume
and increase of interstital fluid volume
- There is little evidence that total-body sodium is increased.
- Lowering hypertensive blood pressures can cause increased kidney sodium retention, counters the drug effects .
-
PIH
- placental vasculitis and ischemia
- increased levels of renin, angiotensin, aldosterone, catecholamines
- generalized vasoconstriction and endothelial damage
- shifts fluid into the extravascular space [DAVp467]
- edema
- hypoxemia (from hypovolemia and decreased CO, tissue perfusion)
- hemoconcentration
- magnesium sulfate
infusion prophylaxsis
-
seizure
- low dose diazepam (valium) 2.5 to 10.0 mg
OK for labor and delivery
[DAVp463]
- larger doses associated with newborn hyptotonia and impaired thermal regulation
- persists for at least a week
- versed has greater fetal effects [MIL p2035]
-
Tachycardia
-
Factors that affect heart rate during neuraxial blockade [FINp196]
- increase:
- volume receptor reflex increases heart rate (from decreased preload)
- decrease:
- baroreceptor reflex slows heart rate
- cardiac sympathetic fiber block slows heart rate
-
vagal tone increase slows heart rate
-
cortical sensory input reduction slows heart rate
- Hypovolemia
- with epidural
- lightening of anesthesia (relative hypervolemia)
- variable relative contributions of decreased SVR and CO to tachycardia from case to case
[FINp196]
- Catecholamine
excess (sympathetic stim)
- Hypercarbia, metabolic substances
-
Intramniotic Infection (Chorioamnionitis)
[NOR p550-54]
-
Clinical signs
- Maternal tachycardia (>100 bpm)
- Fetal tachycardia (>160 bpm)
- Maternal lekocytosis (>15,000)
- Uterine tenderness
- Foul-smelling amniotic fluid
-
Fever response
- Uteroplacental circulation is the more important pathway of heat elimination for the fetus
-
maternal fever is a sign of occult chorioamninitis
- [ISLT] increased fever with epidural contributed by decreased uteroplacental perfusion
- Often associated with dysfunctional labors
- subclinical infection may be present well before symptoms appear
- low-grade infection in the uterus may be detrimental to uterine contractility yet not be extensive enough to cause overt symptoms.
- [ISLT] increased nonselective transfer of materials across the placenta in chorioamnionitis [DAV p462]
-
Syncope
[KAU2 p177-194]
- global reduction in blood flow to the reticular activating system (reversable) [KAU2]
- RAS is the neuronal network in the brain stem responsible for supporting consciousness.
- causes of reduction of cerebral blood flow
- orthostasic hypotension
most common cause [p177] [KAU2]
-
gravity
[KAU2]
- shifts one third of blood volume to lower body decreasing venous return when standing
- carotid sinus BP falls
- thoracic blood volume and arterial pressure are low
-
autonomic reflex dysfunction (neurally mediated syncope NMS, see above)
- hypovolemia (newer finding)
- hypocapnia without systemic hypotension
(low CO2) [KAU2]
- uterus and brain tolerate lower CO2 in pregnancy (max dilated, insensitive to beta2 dilation)
-
epidural increases CO2 in pregnancy
[KAU2]
- decreases uterine blood flow
- effect on brain tolerance [?]
- increased intracranial pressure without hypotension
(CSF) [KAU2]
-
decreased cardiac output
causes decreased cerebral perfusion (pregnancy/ epidural) [p177] [KAU2]
-
other
causes [KAU]
- seizures
- metabolic disorders
- psychiatric disorders
-
Baroreflex
(rapid autonomic reflex) [KAU2]
- AFFERENT
- baroreceptor sensing of low arterial pressure and volume
[KAU, MIL p635]
- sensing inhibited with high epidural in pregnancy
- atrial
- ventricular (fires signal at the onset of ventricular ejection)
- EFFERENT
-
baroreflex
response (rapid autonomic reflex) [KAU2]
- Blood pressure (increase)
- systemic sympathetic neural tone to blood vessels increases (
NE alpha1
)
- increased systemic vasoconstriction
(
raises SVR
)
- systemic sympathetic block gives vasodilation (alpha1 block) [KAU2] [?]
- mid/high epidural in pregnancy also blocks/ vasodilates [?]
- systemic sympathetic adrenal secretion increases (
EPI alpha1
)
- sympathetic renal nerve activity
- with severe hypotension
- adrenal not inhibited with epidural normally [?]
- response to high epidural systemic sympathetic block [?]
- Tachycardia (heart rate increase) [KAU2 p178] ???
- contributions to tachycardia
- sympathetic stimulation
- parasympathetic block
- volume overload (cardiac return)
- increases cardiac output
-
sympathetic cardiac tone increase (
vagal NE beta1
) increases HR
- seen in pregnancy with low/mid epidural sympathetic block
- seen with ephedrine (
direct beta1
)
- parasympathetic cardiac tone decrease (
Vagal AcH ) increases HR
- compensates HR with lo/mid epidural
- lost with hi epidural (sensory block, no reflex slowing)
- net decrease in cardiac output; no net change in HR to bradycardia
- Contractility
- sympathetic cardiac tone increase ( vagal NE beta1 )
- increases cardiac output
-
Venous return
-
Renal nerve
increased sympathetic activity
- direct renal sodium resorption
- indirect renin
, angiotensinII thru juxtaglomerula apparatus from low pressure perfusion pressure
-
Organ system effects
-
abdominal viscera direct effects
-
alpha1 constriction
- beta2 (minimal) vasodilation [p60 tableG&G]
-
Afferent (Sensory) Visceral System
[G&G p56-57]
- most afferent visceral reflexes are mediated thru the CNS
- dorsal spinal nerve root ganglia and sensory ganglia contain sensory cell bodies (synapse outside the CNS)
- non-mylenated afferent fibers are carried into the CNS from the ganglia
- vagus, pelvic, splanchnic, and other autonomic nerves
- 4/5 of the vagal
nerve fibers are sensory (afferent)
-
contain alpha2 receptors
- some afferents are carried in somatic nerves
(synapse inside CNS)
-
muscle blood vessels
-
some integumentary autonomic
- pressoreceptive endings in the carotid sinus and aortic arch and chemoreceptor cells in the carotid and aortic bodies
- afferent fibers pass in the glossopharyngeal and vagus nerves to the medulla oblongata
-
Afferent Receptors
-
Baroreceptors
(
carotid sinus reflex
) [MILp641]
- responds to blood pressure changes
-
mean (integrated) rather than peak effect
- reflex caroticoaortic baroreceptor hi pressure afferent signal to decrease overall CNS
sympathetic tone
and increase vagal tone
that slows the heart
[G&Gp141]
-
arterial
(carotid sinus and aortic arch)
-
increase (
HTN
)
- circumferential and longitudinal stretch receptors
- carotid sinus and aortic arch
- impulses through glossophrayngeal and vagus nerves to nucleus solitarius
- decreases sympathetic activity
- increases parasympathetic activity
- result is decreased heart rate and decreased contractility
-
important at
pressures >170 mmHg
- shifts upward if chronic hypertension
- what if poor LA filling, wide pulse pressure [A?]
-
decrease (
Shock
)
- not functional at pressures <50-60 mmHg
-
venous
(right atrium and great veins) [BAR p125]
- slowing of heart from decreased venous return with spinal anesthesia
-
increased parasympathetic
-
Ventricular receptors
[MILp635]
-
mylenated vagal afferents respond to:
- bradycardia and hypotension
- rate of rise in pressure at onset of ejection
- chemoreceptors
- mechano receptors (constriction of aorta and ventricles)
- sympathetic stimulation
-
unmylenated sympathetic afferents (most) ???
-
Mechano receptors [MILp641]
-
vagus to the brainstem, or dorsal root ganglia to spinal cord
-
Chemoreceptors [MILp641]
-
pH
-
PO2 <50 mmHg
-
carotid and aortic bodies
-
Efferent Systems (Motor/Gland)
- Autonomic systemic efferent synapses are outside the CNS
-
ganglionic plexuses (network routers) synapse with afferent fibers
-
preganglionic neurons to parasympathetic ganglia to postganglionic systems [G&Gp59]
-
ganglia along spinal cord or near organs
-
non-mylenated postganglionic nerves
-
involuntary modulation - unconscious action
-
Sympathetic
Efferent
effectors [G&G p139-142]
-
Structure
- efferent axons synapse with neuron bodies in sympathetic ganglia outside the cerebrospinal axis
- sympathetic nerves ramify with branching distribution
(diffuse discharge is possible)
-
preganglionic
mylenated fibers carried in white anterior rami
-
adrenal medulla
(
T5-T9
)
-
three groups of ganglia
-
paravertebral
-
prevertebral
-
terminal
-
postganglionic
fibers arising from the ganglia are carried in the gray posterior rami
-
synapse with the spinal nerves and effector organs
- all postganglionic sympathetic fibers leave the CNS (
below T1)
-
DIRECT
effects (alpha1, alpha2, beta1, beta2)
- alpha1
POST
synaptic
(
excitatory
)
- smooth muscle vasoconstriction
(pressor effects)
-
blood pressure increases due to alpha1 receptors in the vascular beds. [G&G p140]
- skin vessels
-
gland vasoconstriction
- inhibition of secretion, nasal decongestion, alpha1 effects
- decreases sympathetic and increases vagal central tone by compensatory caroticoaortic baroreflex
[G&Gp141]
- alpha1 block
shifts blood from pulmonary to the systemic vascular bed
[G&G p187]
- alpha2
PRE&POST
synaptic
(
inhibitory
) [p139G&G, MILp261
]
-
PRE
synaptic feedback inhibition
of neural release of NE
(and perhaps AcH)
[G&Gp139]
- blocks NE release
(alpha1, beta1 indirect) and possibly acetylcholine
- cause hypotension and bradycardia
- decreased intestinal motility
- beta blockers may have the same effect
- does not affect baroreflex
- regional anesthetic effect on dorsal horn add to pain inhibition there
-
POST
synaptic
( inhibitory ) [G&Gp139]
- in the uterus
, cerebral cortex, platelets, uterus, parotid gland
- vascular smooth muscle- vasoconstriction
and hypertension alpha2 ???
- alpha2 in the dorsal horn of the spinal cord cause analgesia (as does PRE) [NOR p404]
- beta1
POST
synaptic
(
exitatory
)
- beta1 cardiac
stimulation
- increased contractility (force of contraction)
- increased heart rate
-
adipose lipolysis (release of free fatty acids)
- beta2
POST synaptic
(
inhibitory
)
- relaxation in smooth muscle and glands
(inhibitory) [p139 G&G]
- bronchodilation
- uterine relaxation
- decreased intestinal motility
- vasodilation in skeletal muscles [p140G&G]
- causes systemic vasodilatation, hypotension
- lowers SVR
- inotrope inhibition of neuronal NE reuptake
[MILp553]
-
secretion vasodilation in glands
- gland secretion (insulin)
- causes glycogenolysis and hyperglycemia [NORp645]
- hypokalemia
-
INDIRECT
effect (
alpha1, beta1
)
- norepinephrine store displacement/release from the presynaptic terminal (alpha1, beta1) [p157 G&G]
- in pregnancy, limited indirect beta1 reflex inotropic
activity because of blunting of sympathetic response
- for non-catecholamines that provoke the release norepinephrine, cannot predict precisely the sympathetic effects [p158G&G]
- Parasympathetic Efferent
effectors
-
Efferent structure
- preganglionic fibers are long
- terminal ganglia are near organs in contrast to the sympathetic
- postganglionic fibers are short
- pre to post ganglionic fibers tend to be 1:1 with little branching
-
exceptions like Auerbach's plexus from vagus
- Paraympathetic drugs act on post
junctional receptors [G&G p83]
- AcH parasympathetic relaxant via decreased cAMP [MILp636]
- Protoplasmic bridges communicate impulse between smooth muscle fibers without nerve input
-
Efferent Vasodilation
-
Vagus
contains some efferent fibers (mostly afferent)
- Reflex Parasympathetic
effects
-
compensates for high blood pressure thru the carotiaortic baroreceptor
system
- increase in parasympathetic vagal tone slows the heart
[G&Gp141]
-
alpha1 constriction activity on the vascular beds raises blood pressure
-
reflex increase in vagal tone (parasympathetic) slows the heart
-
lessens the effect of sympathomimetic drugs
- vascular smooth muscle tension lowers sympathetic tone
-
important for drugs with little cardio-accelerator tone (ie, no beta1 or vagolytic effects)
- example phenylephrine (alpha1 agonist)
- used to treat paroxysmal atrial or nodal tachycardia
-
reflexively decreases the sympathetic tone, increases the parasympathetic cardio-decelerator tone
-
slows the heart rate ending the tachycardia.
- in non-neurogenic shock vasoconstrictors are unwarranted, as reflex vasoconstriction mediated by the sympathetic nervous system is already intense [G&G p169]
- in neurogenic shock and shock associated with spinal anesthesia, vasoconstrictors are appropriate as low sympathetic vascular tone
is seen
(low alpha1tone gives vasodilation)
- Sympathetic Drugs [G&Gp144]
- Classes of drugs [DAVp273]
-
alpha agonists
-
phenylephrine
- arterial and venous constriction
- increases venous return (preload)
- low pressure, as CO changes, pressure remains constant
- increases mean arterial pressure (afterload)
- high pressure, as CO changes, pressure changes
-
methoxamine
- pure alpha
- alpha blockers protect against epinephrine induced cardiac arrythmias during anesthesis (such as phenoxybenzamine) [G&G p 148]
- arrythmias potentiated by cholinergic stimulation
-
beta agonists
-
isoproteronol
- increases HR
- increases contractility
- reduces SVR
- no alpha activity
- short half life
-
mixed agonists
(alpha & beta)
-
epinephrine
- beta at low dose
- alpha at high dose
-
norepinephrine
-
sympathetic nervous system neurotransmitter
- alpha at low dose
- aplha/beta1 at high dose
-
no beta2
- increases systolic and diastolic BP
-
maintains or decreases CO as SVR increases
- increases vascular resistance, reduces organ blood flow despite increased MAP
- useful for mild myocardial depression
-
dopamine
- low dose renal and splanchnic vasodilation
- high dose beta effects
-
dobutamine
- beta1, beta2, alpha1
-
ephedrine
[DAVp277]
- noncatecholamine
- releases NE
alpha>beta1
(indirect)
- weak alpha, beta
(direct)
-
Structure activity effects of sympathetic amines
- Sympathetic activity (
maximal potency )
- OH groups
in the 3 and 4 ring positions
of Catecholamines
- especially true for beta
potency
- Epinephrine and Norepinephrine
- Ephedrine has less direct
potency (lacks 3,4-OH)
- CNS direct sympathetic effects
- no Polar groups
increases CNS potency
- no ring OH, no beta carbon OH
- gets into CNS (lipid soluble)
-
EPI, NE have little CNS effects (many OH)
- Ephedrine has moderate CNS effects
(one OH)
- Methamphetamine has high CNS effects (no OH)
-
Peripheral sympathetic effects
-
direct
peripheral activity
(if has polar groups)
- Aromatic ring OH substitution
increases the direct peripheral
potency [p143G&G]
- Ephedrine is less potent direct (no ring OH substitution)
- Beta carbon OH substitution
increases the direct peripheral
potency for a catecholamine
[p143G&G]
- doesnt enter CNS (makes water soluble)
- does not
release norepinephrine (no indirect alpha, beta1(NE)) [p143G&G]
- Side chain polar OH groups increases direct peripheral [p143G&G]
- NE, Dopamine have direct effects
-
indirect
peripheral activity
- if no polar groups, no beta carbon OH
have indirect
peripheral effects only
[G&G p158]
-
indirect
thru NE release from nerve storage terminals (
alpha, beta1 )
- Norepinephrine release from storage sites in the sympathetic nerves to effector organs. [G&G p139, 140, 143]
- nerve ending sensitivity.
- also inhibits NE reuptake, prolonging activity.
- Methamphetamine has very weak
peripheral blood pressure, HR and bronchodilation effects (no OH)
- drugs that lack the -OH group on the aromatic ring but possess a beta-OH group on the side chain (as ephedrine), have the capacity to act both directly and indirectly
to produce sympathomimetic effects [G&G p158]
-
Receptor Selectivity
-
alpha selectivity
is increased with less bulk
on the amino group[G&G, MIL]
- EPI alpha selective
- NE is moderately alpha selective
- Phenylephrine is pure alpha exception despite N-methyl substitution however
-
beta selectivity
increased with more bulk
on the amino group [G&G ch10, MIL]
-
beta2
selectivity if also OH in the 3 and 5 ring position
- less cardiac (beta1)
- more bronchiolar (beta2)
-
Terbutaline has high beta2
-
NE has weak direct beta2 (H on amino group)
- exception is metaproteronol, albuterol
-
Duration of action
- alpha carbon substitution increases
- ephedrine
-
Release of NE
(
indirect
) [G&G p 143]
- EPI, NE, ISO (beta-OH catecholamines) do not release NE
(indirect) and act directly
-
Ephedrine
example
- no ring OH, beta carbon OH
-
alpha methyl substitution increases duration
- Ephedrine has almost exclusive indirect NE release
(despite a beta carbon it is not a catecholamine)
- has weak direct peripheral blood pressure, HR, and bronchodilation effects
(one OH)
- Ephedrine is direct beta1 selective (weak direct beta2)
(no OH) ***
- has weak cardiovascular effects, less than CNS (moderate) at 50mg dose [G&G p143]
-
Sympathetic Drugs
-
Comparison of NE (norepinephrine) vs EPI (epinephrine) vs ISO (isoproteronlol)
-
EPI
-
alpha
-
beta1
-
beta2
-
NE
-
alpha
-
beta1
- (little beta2)
-
ISO
-
beta1
-
beta2
- (little alpha)
-
DA
-
alpha1
-
alpha2
-
EPINEPHRINE
- Actions
- beta (1&2) ( low dose like isoproteronol )
- alpha (1&2) ( high dose like dopamine )
- Cardiac effects [G&G p144,145]
- increases myocardial contraction ( beta1 )
- increases heart rate ( beta1 )
- increases pulse pressure ( alpha1, beta1 )
- mean pressure is not generally greatly elevated (thus little reflex NE) [G&Gp145]
- CO, SV, LV work are increased [p145 G&G]
- cardiac stimulation ( beta1 )
- increased venous return ( beta2 on vascular beds)
- raises membrane potential and increases purkinje conduction [G&Gp147]
- polarizing bias improves depolarized cells
- decreases AV block
- coronary blood flow is unchanged to enhanced by sympathomimetics/epinephrine in man [G&Gp147]
- local metabolic dilation overrides other factors usually
- duration of diastole increases because systole is shortened (beta1) [G&Gp147]
- coronary vessels have primarily alpha receptors (coronary vasoconstriction) in man, but less important
- [ANOTE] coronary flow is more dependent on diastolic coronary perfusion pressure (ie mean) and duration of diastole
- heart rate may decrease at high dose (compensatory vagal discharge) blocked by atropine [G&G p144]
- Vascular effects
- lowers peripheral resistance and diastolic pressure usually [p145 G&G]
- low dose beta2 dominates
- depends on the ratio of alpha to beta response in the various vascular beds
- occasionally there is no change or even a slight rise [p145 G&G]
- sensitivity of beta2 vasodilator receptors over alpha constriction receptors at low doses
- peripheral resistance decreases, due to beta 2 receptors on vessels and skeletal muscle [p145G&G]
- mainly smaller arteriole and precapillary sphincter effects [p145G&G]
- splanchnic resistance decreases
- hepatic blood flow increases (redistribution)
- may cause blood pressure to fall [p144 G&G]
- high dose alpha1, alpha2 dominates
- when alpha and beta are both stimulated, alpha predominates for epinephrine
- increases SVR, BP
- causes vasoconstriction of pulmonary vessels, may cause pulmonary edema [p147 G&G]
- get baroreflex slowing of HR at high doses [p145 G&G] [A?] syncope response]
- causes reduction in circulating plasma volume
- loss of protein free fluid to the extracellular space from increased systolic pressure
- increases erythrocyte and plasma protein concentrations [p150]
- CO decreased like NE
- CNS effects
- little direct CNS effect
- Progress of labor [LEI p1044]
- lumbar sympathetics inhibit labor
- alpha2 sympathetic central inhibition of uterine contractions (NE)
- fright
- higher level than T3
- low-dose lumbar epidural would not affect these sympathetic efferents
- beta2 decreased uterine tone thru sympathetic receptors in uterus
- epinephrine inhibits uterine tone at term ( beta2 ) [p150G&G]
- terbutaline
- beta blocker speeds labor (propanolol)
- pelvic and sacral parasympathetics speed labor
- increase uterine contractions
- block delays the onset and increases duration of labor
- [ANOTE] regional block net effect on labor
- slow labor accompanies low epidural analgesia ("low block", no sympathetic block)
- fast labor accompanies lumbar sympathetic block ("mid block")
- slow labor accompanies hi epidural analgesia ("hi block")
- decreased or increased labor due to sympathetic-to-parasympathetic tone
- rapid cervical dilatation accompanies lumbar sympathetic blockade [LEI]
- leaves accelerator parasympathetic fibers unaffected, speeds labor
- plasma epinephrine level is not the cause of this (lumbar epidural, lumbar sympathetic block both decrease plasma epinephrine)
- Other effects
- muscle contraction
- prolongs the active state of white, fast-contracting fibers
- shortens the active state of red, slow contracting fibers
- [ISLT] EPI makes movements faster, more jerky, less fluid, less range of motion [?]
- blood coagulation accelerates
- WBC count increases, with eosinophelia ([A?] as in stress)
- inorganic phosphate decreases
- potassium rises transiently (released from the liver, taken up by muscle cells)
- augments analgesia (acts directly on alpha2-adrenergic receptors in the dorsal horn of the spinal cord, [NORp404]
- direct vasoconstrictor at low concentration, vasodilator at hi concentration [NORp404]
- Epinephrine-Induced Tachycardia [COL]
- EITR (Epinephrine-induced tachycardic response)
- rapidly develops within 20-40 secs of injection, lasting 15-30 secs.
- blunted in pregnancy and with autonomic blockers
- maternal HR increase of 10 BPM above baseline, within the 1 min of the injection of an epinephrine test dose, is diagnostic of intravascular injection
- sensitivity of 100%
- lasts longer than 15-30 seconds
- quickly returns to baseline
- CATR (Contraction-associated tachycardic response)
- occurs during pain and uterine contraction commonly
-
NOREPINEPHRINE
- Actions [G&G p143]
-
beta1
(= EPI)
-
alpha
(< EPI mostly)
- (no beta2
)
-
Cardiac effects
-
heart rate increases (
beta1
)
- compensatory vagal reflex counters the rate increase
(alpha reflex) [see p145 fig 8-1G&G]
- alpha stimulation increases reflex vagal tone
- vagal baroreflex overcomes the direct cardioaccelerator of NE beta1 [G&Gp152]
- get a slow, forceful heartbeat
[G&G p152,153]
- can even get sinus bradycardia
[MILp635]
-
sympathetic stimulant ( cAMP )
- contractility (CN)
increases
(beta1)
- stroke volume (SV)
increases
-
increases
arterial systolic
, diastolic
, mean arterial pressure
, and pulse pressure
(
beta1,alpha
) [p152G&G]
-
Coronary blood flow
increases
[p152,147 G&G]
- probably due to indirect coronary vasodilation and increased blood pressure (like low epinephrine)
- duration of diastole increases because systole is shortened
(beta1)[p147G&G]
- coronary blood flow depends on diastolic coronary perfusion pressure (mean)
- local metabolic dilation overrides other factors usually (coronary vasodilation)
- coronary vessels alpha in man, but less important (coronary vasoconstriction)
- CO is unchanged or decreased
-
Vascular effects
[G&G p152]
-
TPR
increased (total peripheral resistance)
- marked veno-constriction
,
increasing peripheral vascular resistance
(alpha with no beta2)
-
reduced splanchnic and hepatic blood flow
as mesenteric vessels constrict (alpha1)
-
constricts
muscle blood vessels
(opposite to epinephrine which vasodilates) (alpha1)
- circulating blood volume is reduced, probably due to post-capillary vasoconstriction
(alpha1)
- causes loss of protein-free fluid into the extracellular space
-
EPHEDRINE
-
Actions
- drugs that lack the -OH group on the aromatic ring but possess a beta-OH group on the side chain (as ephedrine), have the capacity to act both directly and indirectly
to produce sympathomimetic effects [p158G&G]
-
weak direct peripheral potency
- absence of polar OH groups on side chain [p143G&G]
- Ephedrine has less direct cardiovascular effects at doses of 50mg
- more central (CNS) sympathomimetic activity (alpha1 & beta1
)
-
crosses blood-brain barrier (non-polar substitutions or unsubstituted)
- so does not decrease uterine perfusion
- indirect peripheral
(
alpha, beta1
)
-
indirect
thru NE release
- acting on nerve ending sensitivity.
- NE release from storage sites in the sympathetic nerves to effector organs. [G&G p139, 140, 143]
- inhibits NE reuptake, prolonging activity.
- stimulates both alpha and beta
receptors (
mixed agonist
)
- alpha1 dyimluant (in non-pregnant)
- alpha1 blunted
in pregnancy
- metaraminol has more alpha1, shows reflex bradycardia to vasoconstriction
- beta1
stimulant
= +++
, useful for moderate hypotension and particularly bradycardia [MILp553]
-
cardiac effects similar to epinephrine [p163G&G]
- less potent
than epinephrine [p143G&G]
-
positive inotrope
- usually no increase in heart rate, unless vagal reflexes are blocked
[G&Gp163]
- increases blood pressure (systolic, diastolic, mean)
- no detrimental uterine blood flow effects
- longer action
- weak beta2 effects [p158G&G]
-
direct
- lung, viscera
, arterioles
(bronchodilator)
- systemic vasodilation, bronchodilation (opposes alpha1)
-
uterus vasodilator
-
indirect
-
inhibition of neuronal uptake of NE [MILp553]
-
indirect
inotropic stimulation thru the inhibition of NE reuptake
(beta2)
- different from norepinephrine which has no beta2
-
Ephedrine has less direct cardiovascular effects
than CNS effects at doses of 50mg
-
more central
sympathomimetic activity ( alpha1 & beta1
)
- crosses blood-brain barrier (non-polar substitutions or unsubstituted aromatic ring)
- usual dose is 2.5 to 25mg IV, or 25 to 50 mg IM
[NOR p553]
-
Vascular effects **
- Ephedrine has a mild pressor
response
-
cardiac stimulation, provided that the venous return is adequate
- mycardial contraction force
increased
- cardiac output augmented
[p163G&G]
- increased pulse pressure
- ephedrine and pseudoephedrine do not raise blood pressure
at doses used for decongestant
- redistribute blood flow to the heart and causes cardiac stimulation
[G&G p168]
- CO (beta1)
- SVR (alpha1)
- HR (beta1 sympathetic tone, if lack of vagal tone )
-
blood pressure increase
- increased systolic blood pressure
- increased diastolic blood pressure (usually)
- increased mean BP (proportional to cardiac output [HUR p 2391]
- partially due to vasoconstriction
- part of peripheral effects due to release of NE (indirect)
- increases
peripheral resistance (TPR apha1)
- renal, splanchnic blood flow
are decreased, (but increases perfusion pressure
) [p163,146G&G]
- [ISLT] is important for uterus which is pressure dependent flow in pregnancy
- coronary, cerebral, and muscle blood flow increase
- slows the heart
thru reflex vagal NE
- reflex caroticoaortic baroreceptor signal increases [p141G&G]
- decreases overall sympathetic tone
- increases vagal tone
- slows the heart
- heart rate may be unaltered, or increased if vagal reflexes are blocked
[p163G&G]
- phenylephrine used in this way to end paroxsysmal atrial or nodal tachycardia [p170G&G]
-
CNS
effects of Ephedrine
- Ephedrine crosses the blood brain barrier, increasing central nervous system activity (it is a lipophilic
compound, with fewer polar OH). [p143G&G]
- Ephedrine has more direct CNS than cardiovascular effects at doses of 50mg
[G&G p143,p138]
- respiratory stimulation
- [ANOTE] may counter epidural induced hypoventilation
- reduction in appetite
- increased wakefulness
- psychomotor activity
- Ephedrine is considerably less potent than methamphetamine
, which is less potent than epinephrine
as a CNS stimulant. [p143,163G&G]
- lack of beta carbon OH decreases CNS activity, increases peripheral alpha, beta activity [p143G&G]
- lack of -OH's makes less lipid (thus CNS) soluble
- "a dose of 50 mg of ephedrine elicits central CNSeffects without inordinate cardiovascular effects". [p143G&G]
- Ephedrine is more powerful in dilating bronchioles and increasing BP and heart rate than methamphetamine
- has direct beta2 though (bronchodilation)
- skeletal muscle beta2
- visceral arteriole beta2
- counters alpha constriction
- improves spinal cord transmission [p161G&G]
- dilates pupils (mydriasis), more so in light-colored iris
- phenylpropanolamine similar to ephedrine, but less CNS stimulation
- Labor and Delivery: Ephedrine
- "Intravenously injected ephedrine restored the mean, systolic and diastolic arterial
blood pressures to the preanalgesic value independent of the degree of hypotension,
and was not followed by marked hypertension in any case
during high epidural blockade.
Although the heart rate did not change, the cardiostimulatory effects were more pronounced than after subcutaneous premedication, resulting in increased stroke volume and cardiac output in all groups. Peripheral vascular resistance increased to the pre-analgesic value."
(The changes in central circulation following a small dose of intravenously administered ephedrine
were studied in middle-aged and elderly
patients during high epidural blockade with bupivacaine 0.5% with adrenaline, etidocaine 1% with adrenaline, and etidocaine 1% plain.) [ENG1 p9, ENG p2]
- parenteral administration of ephedrine to maintain blood pressure during spinal anesthesia for delivery can cause acceleration of fetal heart rate and should not be used when maternal blood pressure exceeds 130/80 (MAP=96). [USPDI p656]
- alpha
and beta1
effects from stimulating NE release
-
Uterine contractions decrease (beta2)
- excreted mostly unchanged in the urine [USPDI]
- acidic urine excretes amphetamine [p159G&G]
-
interacts with oxytocin [USPDI]
- [ISLT] counters loss of vagal tone and tachycardia from mid-block
- Pediatric dose is 25mg/square meter of body surface 4 times per day [USPDI]
- The choice of vasopressor is far less important for fetal health than is avoiding hypotension. [PAL p202]
- Although placental transfer of 50mg doses of ephedrine may result in elevated catecholamine levels, this does not affect neonatal outcome [VER p326]
-
Other Sympathetic Vasoactives
-
Phenylephrine
[MILp554]
- pure alpha1
action
- used to slow superventricular tachycardia
- through reflex compensatory bradycardia
action [G&G p141]
- raises blood pressure
- lessens sympathetic cardioaccelerator tone
- increases parasympathetic cardiodecelerator tone
- ends episode of tachycardia
-
Isproteronol
[G&G p143]
- pure beta
-
Dobutamine
[MILp555]
- beta1
effects
- more inotrope than chronotrope
- less alpha1 than NE
- no indirect NE
- lowers filling pressures
- tachycardia does not usually occur
-
Dopamine
[MILp553]
- response variable
- low dose beta1, beta2
- >5mcg/kg/min releases NE, gives alpha and beta1, alpha dominating
-
Glucagon
[G&Gp169]
- increases contractility thru non-beta receptor mechanism
-
Prazosin
[MILp557]
- alpha1 blocker
- fall in peripheral vascular resistance (arterial)
- decreased venous return to the heart
- causes orthostatic hypotension
- usually no increased heart rate
-
Yohimbine
[MILp557]
- alpha2 blocker
- enhances NE since alpha2 inhibits NE reuptake
-
Cocaine
-
potentiates
sympathetic excitation and inhibition [G&G p 307]
- blocks indirect
sympathomimetic effect (NE synthesis)
- inhibits neuronal catecholamine and cogener transport system [G&G p157]
- blocks indirect effects of ephedrine
- systemic sympathetic tone decreased
- potentiates hypotension with regional anesthesia
- facilitates direct
sympathomimetic effect
- blocks the reuptake of catecholamines from the synaptic cleft, enhancing action ()
- local sympathetic transmission enhanced
- [ANOTE] effectively improves local to global transmission (signal-to-noise)
- direct anesthetic
effects on nerves
- acidic urine increases urinary excretion of amphetamine [p159]
- alkaline urine prolongs action
- [ISLT] acidic urine shorten the action
-
Pain Drugs
-
Local/Regional Anesthetics
- General [NORp334]
-
local anesthetics
block sodium channels, slowing depolarization and action potential
- must first diffuse into axon
to access sodium channels from inside
- more lipophilic
(uncharged) agents diffuse faster
- higher lipid solubility of bipuvacaine allows the drug to enter the nerve cell faster [MILp2039]
- protein binding
and low pH
slows diffusion
- local anesthetics are weak bases (pKa>7.0)must become hydrophilic (charged)
to bind to sodium channels after entry
- high pH
speeds the onset (so acidosis delays onset)
- not simple
-
high lipid solubility diffuses away quickly from site shortening duration
-
Lower concentrations
preferentially block pain over motor transmission
- Dilute concentrations of local anesthetic are as effective as more concentrated solutions
- Use the lowest effective concentration of local anesthetic (preferably bupivacaine or ropivacaine) for labor to minimize motor block
- Bupivacaine and Ropivacaine produce less motor block than equally analgesic concentrations of lidocaine or 2-chloroprocaine.
- Dilute, long acting local anesthetic
-
bupivacaine 0.25% or 0.125%
- bupivacaine 0.75% is no longer approved (cardiac arrest)
- T10 block for labor
- 3% 2-chlorprocaine
- 2% lidocaine
- [A?] use of nesacaine
- Cesarian
section
- more concentrated gives a denser block for C/S
- patients are more comfortable when the level of sensory block is higher than T5
[NOR p406]
-
incomplete lower level block of L5 to S2
causes visceral pain from traction on the uterosacral ligaments or bladder during cesarian
- IV injection causes agitation, visual disturbances, tinnitus
-
sympathectomy is typically 2-6 dermatomes above sensory level for spinal, at same level with epidural anesthesia [MILp1496]
-
sympathetic blockade extends variably above the level of sensory block
-
level of sensory anesthesia relates to the degree of hypotension
-
Lidocaine
[NORp124]
- faster onset
then bupivacaine [NORp336]
- least protein bound, more fetal transfer
-
more motor block and less analgesic then bupivacaine at same concentrations [NORp336]
- higher fetal transfer with perineal infiltration
than with epidural
-
no adverse neonatal effects
-
Bupivacaine
[NORp124,p335,p402]
- high lipid solubility
- slow onset
-
long duration
- rapid fetal tissue uptake
-
more sensory than motor block
- addition of opioids to bupivacaine epidurals potentiates the anesthesia, and lowers the concentration of local anesthetic used, producing little or no motor block
- 0.0625% bupivacaine with 2mcg/ml fentanyl showed 97% without motor block when given at full dilatation
.
-
continuing the infusion provided better pain relief without any increased duration of labor [NOR p353]
- most protein bound, less fetal transfer (except acidotic fetus) [NORp119]
-
more cardiotoxic
than lidocaine (binds longer in sodium channel)
- pregnancy does not affect cardiotoxicity
- impairs impulse conduction, but does not affect sinus node
[NOR p604]
-
little significance
because of small dilute solutions with regional anesthesia [NOR p337]
- the clinical importance of these observations about toxicity must be balanced against clinical studies showing limited cardiovascular depression in patients undergoing bupivacaine-induced seizures during regional anesthesia
. [MIL]
-
20ml of 0.125% bupivacaine will provide analgesia in 95% of laboring women
-
no neonatal adverse effects
- Fetal heart rate changes are usually associated with uterine hypertonus,
- probably secondary to a decrease in plasma catecholamine
concentration associated with the onset of analgesic.
- may lead to increased uterine tone, with decreased placental perfusion and fetal asphyxia.
- Catecholamines have a tocolytic effect
- [A?] sympathetic adrenal medulla block?
- Fetal heart rate changes likely not
due to direct drug effect on the fetal heart
- bupivacaine has reduced protein binding and higher free levels, with enhanced toxicity from progesterone [MILp2040]
- bupivacaine and ropivacaine have similar characteristics, with a slower onset time and longer duration than lidocaine [MILp2048]
- caudal spread does not diminsh with time, a property that may be an advantage compared to ropivacaine in long labors [NOR p125]
-
Ropivacaine
[NORp125, p337, p402, p404]
-
low lipid solubility
- pure S-enantiomer
- similar to bupivacaine in structure and in clinical reports, with slower inset and longer duration than lidocaine. [MILp2041]
- similar sensory block to bupivacaine
- in equal concentrations, similar duration than bupivacaine
-
less potent (50%) compared to bupivacaine
-
15 to 30 ml of 0.5% local ropivacaine is required (70-150mg). [MILp2041]
- less motor blockade- some evidence of fewer instrumental deliveries
- would expect bupivacaine to produce more motor block and analgesia for the same mg dose.
- shorter duration of motor block with ropivacaine (for same concentration)
- some limitations of these studies
- in vitro studies suggest reduced blockade of motor fibers compared to bupvacaine, but studies in laboring patients have yet to confirm this. [MILp2041]
- addition of opioids to bupivacaine epidurals potentiates the anesthesia, and lowers the concentration of local anesthetic used, producing little or no motor block. similar studies are needed with ropivacaine.
-
less effective in a long labor (
caudal spread decreases with time
)
- more cardiotoxic than lidocaine, less than bupivacaine at same mg dose
[OMO]
- Ropivacaine has a CNS-to-cardiotoxicity ratio intermediate between lidocaine (less) and bupivacaine (more). [MILp1513, 2041]
- cardiotoxicity not
enhanced by progesterone. [MILp2041]
- cleared more slowly from plasma, maternal and fetal plasma show 2X higher concentration [NOR p125]
- no effect on uteroplacental or fetal circulation
- crosses placenta
similar to bupivacaine
- added epinephrine has no effect on anesthesia [OMO]
- [ANOTE] ropivacaine is a direct vasoconstrictor
-
Ropivacaine in Obstetrics, Rudolf Sienstra MD, PhD
, Leiden University Medical Center, Leiden, Netherlands
www.esraeurope.org/abstracts/abstracts98/stien1.htm
- ropivacaine has a greater separation between sensory and motor blockade, especially at lower concentrations
-
less intense motor blockade of shorter duration with epidural blockade
-
duration
of sensory block is shorter for ropivacaine, indicating a lower potency
- dose response curve of epidural ropivacaine is shifted to the right when compared to epidural bupivacaine
- especially regarding motor block, and to a lesser extent sensory block
-
slower uptake into nerve cells means delayed onset, less potent in shorter procedures
- [ISLT] greater separation between sensory and motor blockade would also mean greater separation between sympathetic and sensory or motor blockade, but we dont measure it
-
major systemic toxicity is cardiotoxic, but less so with ropivacaine
- other studies
-
ropivacaine 0.2%, best to use infusion rate of 6-8ml/hr for labor (12-16 mg/hr) [behamou]
- meta analysis of prospective studies
-
ropivacaine and bupivacaine are equally efficacious regarding pain
relief. ropivacaine and bupivacaine were "equally effective and clinically indistiguishable" at 0.125mg concentration [owen et al]
- "a significant difference in the incidence and intensity of motor block did not result in differences in the incidence of spontaneous and instrumental deliveries,
contrary to the widely held opinion that a reduction in motor block will increase the number of spontaneous deliveries."
- with ropivacaine 0.75%, 50% of the women had an unneccessarily high level of sensory blockade
[irestedt]
- only 6 of 32 (19%) had adequate anesthesia with similar dosing
[morton et al] ???
- visual analog scale for pain is flawed (VAS)
- values have only a semiquantitative association with pain at best
- similar reduction in VAS-scores does not necessarilty represent similar pain relief
- participants in the study may become eager to please, with placebo effect confounding
- opioid enhances the pain relief, allowing for reduction in dose and reducing motor block incidence with bupivacaine
- studies comparing to ropivacaine are lacking
-
Ropivacaine in post-operative pain management, Dr. Finucane, Vancouver, Canada
www.earaeurope.org/abstracts/abstracts98/finucan2.htm
- ropivacaine has lower lipid solubility
(hydrophilic)
- marker for
- lower potency
- lower toxicity
- lower motor block
-
comparison to bupivacaine in equal milligram doses
- equipotent with bupipvacaine for infiltration blockade
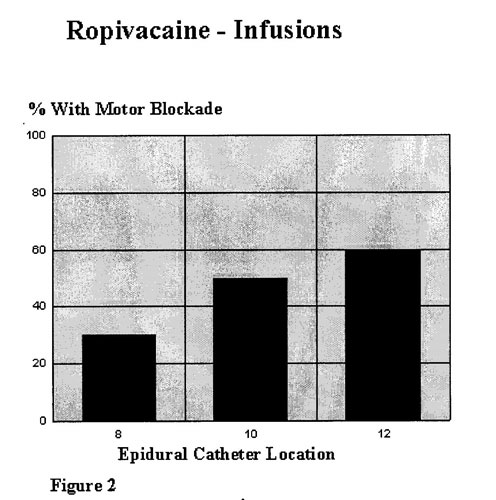
- equipotent with bupivacaine for peripheral blockade
- less potent than bupivacaine for central neural blockade
- requires 150% mg for mg
-
motor blockade (ropivacaine 1,2,3 mg/ml compared to bupivacaine 2.5mg, and saline)
-
motor blockade increases with increasing ropivacaine concentration
- barely measurable motor blockade with ropivacaine 1mg/ml
- most intense motor blockade with bupivacaine 2.5mg/ml
- motor block resolved more quickly with ropivacaine (sensory also shorter duration)
-
motor block increases as level of block decreases
-
(50%) with lumbar placed catheters
, (10%) with thoracic catheters (2mg/ml)
- see diagram for level of catheter effect (2mg/ml)
-
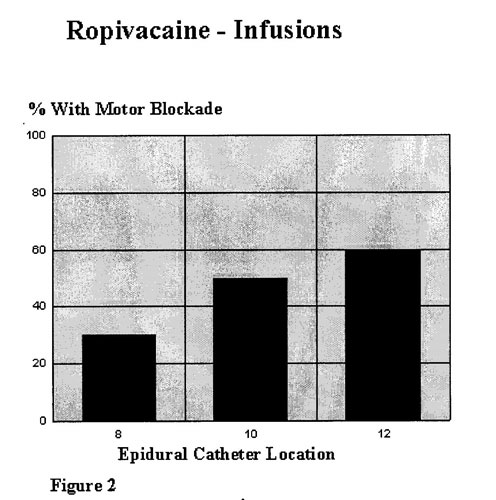
-
[A?] important for obstetric perineal anesthesia
- addition of fentanyl
to ropivacaine enhances pain relief
- also increases the incidence of adverse events
-
delays readiness for discharge.
-
Ropivacaine in Obstetric Anesthesia, Stephen Gatt
www.manbit.com/oa/c4.htm
- ropivacaine has lipid solubility between lidocaine(low) and bupivacaine (high)
- hydrophilic
- more than lidocaine, less than bupivacaine
- ropivacaine is highly plasma protein bound
(94%)
- ropivacaine is rapidly cleared
from the plasma
- duration of action and onset time are similar to bupivacaine
- may be due to ropivacaine has mild vasoconstrictive
properties, and does not require the addition of epinephrine
- it is a short acting anesthetic (short half-life), and effect wears off quickly once it is cleared from the site
- no other receptor affinity
- histaminic
- seratoninic
- alpha
- beta
- muscarinic
- at low concentration, ropivacaine has less motor blockade because of less effect on large motor fibers (A-fibers)
-
delayed entry into large cells
delays and lowers the peak effect but lasts longer
relative to smaller fibers
- concentration surface to volume area
- effects are a function of time so misleading
- ropivacaine has less CNS effects (lightheadeness, tinnitus, tongue numbness)
- pregnancy does not affect CNS, cardiac toxicity
- [ISLT] may have a greater sympathetic block than would be expected for the same amount of sensory, CNS effects
- bupivacaine:ropivacaine arrythmic dose = 2:1
- would expect 1.5:1
when adjust for relative potency
- NACS (neural and adaptive scores) of neonates need to be adjusted for total potency, not mg dose
- slightly better for ropivacaine before the adjustment with 0.25%
- concentration effect/ equipotent [?]
-
Experience with ropivacaine for labour analgesia, Genevieve Goulding
www.manbit.com/oa/c116.htm
- worldwide double blind comparing ropivacaine and bupivacaine
-
most anesthestist regimens
-
bupivacaine 0.25% with 75-100mcg of fentanyl to intiate block
-
bupivacaine 0.125% with fentanyl 5mcg/ml for continued infusion
- many of the regimens evolved by trial and error
- consider using a more potent agent for mid-forceps delivery
- In some centers, patients receiving ropivacaine were noted to have less motor block
- however, this difference was statistically significant only in one group.
- ropivacaine required more frequent top-ups without fentanyl
- breakthrough pain" is usually due to a low level of block on one side
- usually responds to a bolus
- persistent low back pain or deep perineal pain remains a challenge
- important for obstetric anesthesia for perineal anesthesia [?]
- [ISLT] larger fibers are resistant to ropivacaine in the lumbar and sacral regions
-
General Anesthetics
-
Halothanes
-
Baroreceptor-Sympathetic reflex (
BSR
) [SAE]
- Halothane anesthetics attenuate response to change in BP
- did not alter aortic nerve activity (
afferent
), indicating that anesthetics did not alter wall baroreceptor sensitivity
- suppressed the sympathoinhibitory response (efferent arterial)
to aortic stimulation at 1.0MAC
- implies that the reflex supression by the anesthetics is mediated by supression of the central or peripheral sympathetic integrating system
- renal medulla sympathetic (efferent) nerve activity (RNA) is decreased by enflurane at 1.0MAC, but not by sevoflurane and isoflurane
-
halogenated hydrocarbons sensitize the heart to the arrythmic action of catecholamines and related drugs [G&Gp169]
- sevflourane is category B in pregnancy, investigated in rats and rabbits but not humans [NOR p166]
-
Narcotic Analgesics
-
Narcotic parenteral analgesia
[THOp785]
-
may result in slightly more sedated newborns, but not usually of clinical significance
- average total dose 140mg (demerol)
- opioids and propofol linearly decrease the vasoconstriction and shivering thresholds
- Morphine
[NORp258]
-
parenteral
- causes excessive maternal sedation
- decreases FHR variability and may lower baseline FHR
- neonates are very susceptile to the respiratory depressant effects of morphine, especially if premature (more than merperidine)
- [ISLT] oxycontin is similar to morphine (preadmission drug use)
- epidural [NORp405]
- not lipid soluble
- slower onset
- plateaus at 3.75mg
- longest lasting
-
Meperidine (Demerol)
[NORp126]
-
Parenteral
- decrease in fetal heart rate variability during labor, with CNS depression
- normal variability during stimulation like fetal movement or contractions
-
less neonatal respiratory depression
- neonate can metabolize
- Longer drug to birth interval
has more effects on the neonatal neurobehavior
- Metabolites have long plasma half-life
.
- fetal drug level increases over time > maternal
-
may interfere with breast-feeding
- Nalbuphine (Nubain)
[NORp260]
-
Parenteral
-
fewer maternal side effects [NORp128]
-
plasma half-life is 5 hours
(long) [NORp260]
-
FHR change is similar to meperidine [NORp128]
- fewer spontaneously reactive episodes, although does not affect vibroacoustic stimulation [NORp128]
- causes neonatal respiratory depression
[NORp260]
- pain relief plateaus at >10-20mg, little pain imporvement with higher dosing
- neonates have lower neurobehavioral scores
than with merperidine [NORp260]
-
neonate can't metabloize
- completely reversed with naloxone, but requires continued dosing
- Butorphanol (Stadol)
[NORp260]
-
Parenteral
-
fewer maternal side effects [NOR p128]
-
less maternal respiratory depression
with higher doses
-
peaks at 30-60mins
- FHR change is similar to meperidine [NOR p128]
- fewer spontaneously reactive episodes, although does not affect vibroacoustic stimulation [NORp128]
-
Fentanyl
[NORp126]
-
Parenteral
-
excellent labor analgesia
- more lipophilic
and higher protein binding
than meperidine
-
short plasma half-life (rapid tissue uptake, multiphase elimination)
- decrease in fetal heart rate variability for 30 minutes when IV.
- Low neonatal blood levels after two hours
-
Neonatal scores do not differ from control infants
-
Regional
-
Improves epidural anesthesia without neonatal effects at c-section
-
limit epidural fentanyl to 3mcg/ml
to avoid itching [NORp338]
- concentration dependent [?]
- limit spinal fentanyl to 15mcg
to avoid itching, and significant maternal sedation and hypotension
- severe respiratory depression or respiratory arrest rarely
after intrathecal fentanyl [NOR p606]
- often these patients also receive parenteral opioids.
- nalaoxone reverses the effects
-
Sufentanil
[NORp127]
-
Parenteral
-
very short plasma half-life
-
not detected in fetal plasma
-
no MAP, heart rate, acid-base or uterine blood flow effects in Mom or fetus
-
expensive
- sufentanyl has less effect on fetus because of larger volume of distribution
[NORp338]
-
sufentanil is recommended over fentanyl by Norris
-
Regional
-
the maximum safe dose of intrathecal sufentanil in laboring women has yet to be determined. [NORp607]
-
see page 339 table4 outline of epidural doses
-
Alfentanyl
[NORp127]
-
no
confirmed advantages
- Regional
- neonatal hypotonia after labor epidural [NORp127]
- large doses (30mcg/kg) produce neonatal hypotonia [NORp405]
-
Benzodiazapines
[NORp123]
- oral administration produces poor suckling
- IV administration may cause fetal hypotonia and hypotermia
-
low dose diazepam (Valium) 2.5 to 10.0 mg
is OK for labor and delivery [DAVp463]
- larger doses associated with newborn hyptotonia and impaired thermal regulation
- persist for at least a week
- Versed
has greater fetal effects [MIL p2035]
- Ambien
activates benzodiazapine receptors although not a benzodiazapine
-
Muscle relaxants
-
Succinyl choline
- "to date (1999) no nondepolarizing muscle relaxant can completely match the onset and rapid recovery of succinyl choline when used for intubation in the pregnant patient." [NOR 124]
- transfers rapidly to the fetus (5-20% of maternal)
-
Hypnotics
- Propofol
[NOR p386, p122]
- Propofol offers no advantage over Thiopentol
for general anesthesia
- unpredictable hemodynamics
- neonatal effects of propofol are unclear
- propofol depressed 1 and 5 min Apgar scores
-
shortest induction to delivery time (no mixing time)
-
inhibits unterine contraction ([A?] affects blood loss)
- opioids and propofol linearly decrease the vasoconstriction and shivering thresholds
-
"On balance, there is no compelling reason to routinely use propofol as an induction agent at cesarian delivery." [Nor p123]
- Propofol infusions have been used to maintain anesthesia with or without nitrous oxide. "This technique seems to have no significant advantage
and is of increased cost as compared to traditional methods".
-
PREGNANCY
-
Drug metabolism in pregnancy
[NORp116]
- Larger volume of distribution
- Higher renal clearance/ GFR
- Lower Serum albumin reduces the number of albumin binding sites
-
i
ncreases the potency of protein bound free fatty acids and acidic drugs
.
-
Placental transfer
[Nor p116-129]
- mostly by simple passive diffusion
-
factors
- low
protein binding
- high
lipid solubility
- bupivacaine
- low
molecular weight (<600)
- low
degree of ionization
-
muscle relaxants dont cross (water soluble)
-
hydralazine crosses the placenta [NORp98]
-
transfer of weak bases across the placenta
- Fetal hypoxia
and acidosis increase
transfer
-
Fetal acidosis increases the effects of local anesthetics (since weak bases)
-
local anesthetics are weak bases (ropivacaine)
-
placental damage
- hypertension, diabetes, PIH
- all damage the capillary integrity of the placenta, resulting in nonselective transfer of materials across the placenta
- [ISLT] that chorio could also be a factor in labor with increased transfer of local anesthetic (ropivacaine)
-
CSF
has lower density in pregnancy [NOR p21]
- Intrathecal drugs spread further in pregnancy
- Progesterone [NOR p20,21]
-
increases during pregnancy
-
speeds the elimination
of some drugs by inducing hepatic metabolism, but others inhibits
- Progesterone decreases free thyroxine level
[NOR p20]
- HCG stim effect in early pregnancy maintains early thyroid production (peaks in second trimester)
-
free thyroxine level (FT4) falls in third trimester, progesterone may be causative
- Prolonged (4day) exposure to progesterone makes nerve fibers more susceptible to local anesthetics
- require less local anesthetic dose
- [ISLT] PMS has depression effects
-
Inhalation anesthetic MAC
- Isoflurane, Enflurane, Halothane MAC is lower in pregancy (0.78%)
-
Glucose
-
maternal dextrose infusion decreases umbilical artery pH and worsens the fetal response to hypotension. [NORp422]
- IV solution for regional anesthesia shoud not
contain dextrose. Rapid dextrose infusion produces maternal hyperglycemia, hyperinsulinemia, and an increase in blood lactate. Neontatal hyperglycemia and then hypoglycemia follow shortly after delivery.
[NOR p408, Philipson 1987]
- high-carbohydrate
snack or alcohol
usually lowers nocturnal blood pressure
- DONT BOLUS WITH GLUCOSE
- Cardiovascular changes in Pregnancy
[NOR p3]
-
Pregnancy hormones
- Even a brief exposure to Estrogen
causes the cardiac changes seen in pregnancy [NOR p5]
- in sheep, infusing conjugated estrogens for 4 hours
elevates CO (32%) and HR (50%), and lowers MAP (-10%) and SVR (-19%).
-
Relaxin
increases HR, left ventricular systolic pressure, and contractility in rats [NOR p5]
- like NE effects (beta1)
- Plasma Progesterone
concentration progressively rises throughout pregnancy. The time course alone makes progesterone a likely mediator in many physiologic alterations seen in pregnancy. [NOR p20,30; G&G p1436]
- supresses uterine contractility
- inhibits the function of T lymphocytes
- endometrial/placental vasculature
-
Systemic baseline pregnancy changes
[NOR p30, HUR 2391-3]
-
(
SVR
) Systemic Vascular Resistance
decreases
throughout pregnancy [HUR 2391]
- falls to one-third
its prepregnancy value by 20 weeks
- then rises gradually, returns to normal only a few weeks after delivery
- (
TPR
) Total Peripheral Resistance decreases 15%
- (
PVR
) Pulmonary vascular resistance decreases (-35%)
-
-
(
MAP
) Mean arterial pressure
decreases (15mmHg)
- decrease in Diastolic Blood Pressure (DBP) -10 to -20 mmHg
- increased venous bed dilation (20 weeks on) [HUR p2391]
- venous dilatation pools blood, lowering venous return (VR)
- venous constriction would increase VR
- modest
decrease in Systolic BP (SBP) up to 15mmHg in 2nd trimester
only [MOB]
- gradual increase
to non-pregnant BP by term
- (
HR
) Heart rate increases gradually (to 25%) above nonpregnant by delivery
- in labor rises 34% with each contraction
-
(
SV
)
Stroke volume increases
(30%)
- (SV) decreases again by the 20th week due to vena cava obstruction
and increased venous bed dilation
.
- (VR)
venous return impaired by the enlarging uterus copressing the aorta and vena cava, especially when supine.
- heart has to enlarge (no change in ejection fraction)
- in labor increases with each contraction (500ml)
-
(
CO
) Cardiac output
increases (40%) [NOR p8; HURp2391,1061]
- Cardiac output in pregnancy is increased primarily from stroke volume
, not heart rate or inotropy. [WILp206]
- peaks in the late 2nd trimester, and returns to nonpregnant levels just after delivery
- directly related to the mean blood pressure
, inverse to the SVR
- CO, SV, HR all decrease in the supine
vs lateral position in labor
- fall in CO by position compared to left lateral [HURp2390]
- supine
0.6 L/min lower
- standing
1.2 L/min lower
- venous return is important
-
labor increases CO
-
marked elevation of CO following delivery
-
epidurals decreases CO when drop in systolic blood pressure >25% (<90 mmHg) [FINp197]
- no change to increase otherwise [NOR p10]
- variable SVR vs CO effects depending if surgical or non-surgical [FINp197]
-
(
VV
) Vascular volume
increases
(35-45%)
- sodium and water retention (stimulated by estrogen)
- fall in SVR (arterial dilation)
- pooled in the great veins of the pelvis and lower extremities (venous capacitance)
- hematocrit decreases from hemodilution
- colloid osmotic pressure is lower (-28% at term)
- the distribution of blood flow is not fully understood
, and is affected by changes in local vascular resistance.
-
(
APP
) Arterial pulse pressure
increases
[HURp256]
-
Pregnancy
can produce an increase in arterial pulse pressure
due to an increase in stroke volume
and ejection velocity
- diastolic lowers more, then increases less than systolic in pregnancy
- increased pulse pressure with increased intravascular volume
- often with a decrease in peripheral resistance
(TPR)
- also seen with epidural ([A?] helps maintain mean BP and CO)
- with decreased catecholamines
- ( IVC) Inferior Vena Cava
pressure increases [NOR p21]
- ( CVP/RAP ) essentially no change (
-2%
) [NOR p10, HUR p1061]
- CVP does not change appreciable between late pregnancy and the puerperium. [WILp208]
- Central venous pressure (CVP) rises in the first 24 hours post delivery if oxytocin is given
- Epidurals decrease CVP often without affects on maternal heart rate
- ( COP )
Colloid Oncotic Pressure decreases (-14%)
-
Arterial blood pressure
- "BP in the brachial artery does not provide a reliable estimate of the pressure in the uterine or other arteries that lie distal to aortic compression."
[WIL p 210]
- with systemic hypotension, as occurs with spinal analgesia, the decrease in uterine artery pressure below the level of aortic compression is even more marked than in arteries above
[WIL p210]
- when supine, uterine artery pressure is significantly lower than that in the brachial artery
[WIL p210]
- Supine Posture in the pregnant women affects arterial blood pressure
- Blood flow in the legs is impeded in the supine position [WILp209, fig 8-13 p210]
- Femoral venous pressure rises by a factor of 3 in the supine position [WILp209, fig 8-13 p210]
- Antecubital venous pressure is unchanged with position
- Leg MAP or arterial flow is unchanged with position [NOR p7]
-
Treatment of hypertension in pregnancy is for the benefit of the mom, not the fetus
[see WIL p733].
- treat acutely when maternal diastolic
pressure reaches 100mmHg, to prevent hypertensive vascular damage (lower to 90 -100) [WILp734] ???
- treat with chronic HTN when BP>
150/110, if not already on medication [WILp735]
-
Blood pressure in pregnancy [BSOG p69]
-
systolic
BP changes little in pregnancy (dip 2nd trimester)
-
diastolic
BP is reduced in the first two trimesters, normal in the third
-
venous
BP in the legs is increased during pregnancy
- uterus causes mechanical obstruction
- high pressure venous outflow from the uterus
-
placenta acts as an AV shunt
- increases CO
- acts to decrease systolic BP and pulse pressure, balances increased contractility and HR
-
vascular responsiveness
- pregnancy blunts sympathetic vasoconstriction (alpha1) and vasodilation [NORp7] ???
- pregnancy blunts parasympathetic responsiveness, particularly in the 2nd trimester. [NOR p7]
- pregnancy blunts non-sympathetic pressors vascular constrictor response
(AII)
[NORp91]
- pregnant women are refractory to the pressor effects of angiotensin II. [WILp 208]
- progesterone metabolite 5alpha-dihydroprogesterone or theophylline
restores the lack of refractoriness in PIH patients.
- pregnancy inhibits the chronotropic response to isoproterenol (beta1) to a marked degree.
-
less reflex tachycardia
-
may be a pregnancy related circulating factor [NOR p8]
- epinephrine (alpha, beta agonist) does not consistently produce maternal tachycardia in pregnant women. [NOR p602]
- limits the precision of an epinepherine test dose in pregnancy
- [ANOTE] why ephedrine has inotropic rather than chronotropic effect
[NOR p8]
- pregnancy attenuates adrenal catecholamine (ADR)
secretion in response to stress
-
pregnancy blunts increased HR
that with increased vascular volume [NOR p7]
-
Uteroplacental vasculature [NOR]
-
uterine blood vessels are maximally dilated
during pregnancy ???
- Increased placental vascular resistance, which is ordinarily low, will be detected by a decrease in diastolic blood flow through the umbilical artery.
- fetal umbilical artery bloodflow ultrasound velocity waveforms reflect placental (fetal) vascular resistance [NORp621-22]
- This technique of umbilical velocimetry is underutilized in routine clinical practice.
- decreased diastolic flow is reflected in an increase in Pulsatility Index (PI)
- The Pulsatility Index (PI) is the ratio of systolic to diastolic blood flow velocity (S/D ratio)
- utero-placental circulation is maximally vasodilated
at term [NOR p113]
- these vessels can't dilate further in response to decreased aortic blood flow or increased fetal metabolic demand, unlike other vascular beds that undergo autoregulation [NORp620, p113]
- uterine artery maintains its normal constriction and dilation properties in pregnancy [NORp8] ???
- alpha agents constrict the uterine arteries and impair uteroplacental blood flow
- makes beta adrenergic agents preferable for the treatment of hypotension.
- uterine blood flow depends on maternal blood pressure [NOR p113]
- Hypotension, decreased maternal cardiac output due to aorticaval compression, sympathetic blockade, or hypovolemia directly decreases placental perfusion. [NORp620]
- Flow can increase, but only from increased maternal arterial pressure.
- Uterine blood flow falls if redistribution of total flow is required by the mother, or if there is a fall in maternal blood pressure and cardiac output. [WILp2391]
- also have direct AV shunts
- intrauterine pressure from contractions can decrease placental blood supply [NOR p113]
- uterine contractions
also transiently decrease intervillous bloodflow
in proportion to their duration, intensity, and frequency, because blood supply to the placenta crosses the myometrium, [NORp621]
- uterine blood flow
- decreases during maternal hypotension
(sympathetic block, hypovolemia, hemorrhage, compression of the inferior vena cava) or by increased uterine vascular resistance either directly to changes in vascular tone or indirectly by altering uterine contractions or uterine muscle tone [MILp2030]
- sympathetic block
- reduces uterine blood flow thru decreased perfusion pressure in animals
- low sympathetic block
- allows reflex sympathetic cardiostimulation
- inhibits vasoconstriction of the lower body
- gives tachycardia and decreased venous return (hypotension)
-
high sympathetic block
- inhibits reflex sympathetic cardiostimulation
- hi spinal block (T1-3) produces bradycardia by blocking the cardioaccelerator nerve fibers, allowing vagal inhibitory tone to dominate [MORp405]
- inhibits sympathetic vasoconstriction of the upper and lower body
- gives bradycardia and decreased venous return (hypotension)
- Cesarian cardiovascular effects
[NOR p8]
-
CO, SV, HR
- change less than with vaginal delivery
- greater blood loss with cesarian explains these differences
-
Type of anesthesia does not affect maternal cardiac parameters
-
Hyper/Hypoventilation in labor
- pain of labor induces maternal hyperventilation
- pain from episodic uterine contractions
produces corresponding increase in minute ventilation
. [MIL p2025]
- maternal hyperventilation lowers pCO2
, which transfers carbon dioxide from fetus to mother [NORp116]
- results in maternal hypocarbia and alkalemia
- 6-7mmhg
-
maternal hyperventilation probably produces
fetal hypoxia [NOR p16]
- hypocarbia
can lead to hypoventilation between uterine contractions, resulting in intermittant maternal hypoxia
-
Oxygen saturation fell below 90% in 49% of laboring women
- particularly in obese and with parenteral medications
- uterine blood flow decreases if PCO2 drops too low
-
hi maternal paO2 does not change fetal pH, so oxygen is safe [NOR p16]
- [ANOTE] ?effect of low maternal paO2 on fetal pH, particularly intermittant, probably not significant
- epidurals limit minute (hyper) ventilation, and the accompanying hyper/hypo ventilation cycle in labor [MIL p2025, NOR p15, p116]
- maternal hypercapnia (hi pCO2) may increase uterine blood flow, actually increasing fetal oxygen supply thru increased cardiac output (if mom is not hypoxic herself)
- [ISLT] maternal PCO2 increase with epidural accounts for lower pH/ fetal acidemia seen with epidural at cesarian
- [ISLT] hypocapnic mothers (PCO2 <17 mmhg) offset fetal acidosis, without fetal hypoxia if mom's blood is adequately oxygenated ???
- [ISLT] trade off of fetal hypoxia versus fetal hypercarbia
- [ISLT] since fetus is in a low oxygen tension state anyway, Hi CO2 (LOW pH) may be the more important parameter (infant has to get rid of CO2 from anerobic metabolism if low oxygen)
-
Vascular occlusion effects in pregnancy
[NOR p595]
-
Overview
- Aortic occlusion
- ( in
all positions
,
with contraction
)
- Aortal compression is not dependent on postion
- Aortic occlusion occurs almost exclusively during contractions
- The uterus squeezes the aorta during contractions in up to 86% of laboring women
- Aortic compression by the gravid uterus may leave unchanged or increase maternal brachial artery blood pressure (upper body) by increasing systemic vascular resistance, while reducing uterine blood flow/pressure (lower body). [NORp624]
- Aortic compression is more frequent
- if the cervix is dilated less than 5cm
- if the fetal head is not engaged
in the pelvis
- if the fetal head is occiput posterior
- Aortic compression summary
- upper body artery blood pressure is not
lowered
- lower extremity blood pressure
& flow decreases, including to the uterus.
- aortic
compression during contractions
- aortic
compression does not respond to position
change
- Venous occlusion
- ( in
supine position
, without (between) contractions
) [NOR p595]
- Inferior Vena cava occlusion/obstruction is position dependent
- The more posterior vena cava is compressed by the uterus in the supine position
- right or left lateral position relieves caval compression
- more frequently between contractions [see p594 fig1]
- this worsens as the pressure within the vena cava falls (hypotension) [NORp595]
- Inferior vena cava compression
decreases venous return
to the heart
- reduces right ventricular preload and maternal cardiac output [NORp624]
- causes maternal uterine and lower extremity hypotension
-
reduced pulse pressure
in the lower extremities and uterus (systolic and not
diastolic BP
) from aortocaval
compression [see p594 fig1]
- Venous compression summary
- decreases venous return, decreases preload (volume)
- lowers BP and CO in all arteries and veins
- decreases lower extremity blood pressure/flow below compression
- venous
compression occurs mostly between
contractions
- venous
compression responds to position
change (better in lateral)
- No anesthesia
/ Supine position /
Vascular Obstruction Effects
[NOR, HURST
]
-
Maternal cardiovascular parameters
-
CO
, SV
, Systolic and Diastolic BP
(SAP/DAP) decrease in the supine
compared to lateral position
- Vena cava is obstructed
by the enlarged uterus (20 weeks on) [HUR p2391, NOR p6]
- venous return (VR) decreases, decreasing right atrial pressure (RAP), which limits SV and CO
- hypotension follows unless compensatory tachycardia or peripheral vasoconstriction ensues
- 15-20% of third trimester patients show hypotension or tachycardia while supine
- regional or general anesthesia compromise the gravida's ability to compensate for a fall in venous return.
-
SVR increases
significantly while supine
- this helps maintain Systolic Blood Pressure and tissue perfusion
-
HR increase
(mild) offsets
changes in CO
- left lateral has the lowest heart rate
- [see fig 3a p6 NOR]
- Circulation loop
- high pressure
- aorta
- precapillary
- capillary
- low pressure
- post capillary
- vena cava
- right atrium
- lung
- left atrium
-
Without
Contractions
(
no anesthesia
)
-
(IVC) compression
[NORp6]
-
at term, gravid uterus commonly obstructs the Inferior Vena Cava (IVC) completely where it bifurcates [NORp6]
-
infrarenal vena cava
-
blood instead returns to the heart thru dilated azygous and vertebral (epidural) veins [NORp6]
-
decreases venous return
- decreases right atrial pressure
, SV
and CO
(from obstruction to return flow)
[NORp6]
- increases HR
to compensate
-
raises venous
systemic pressure [NORp6]
- confusing because circulation is a loop
- raises lower body venous pressure (systemic) before
obstruction (between capillaries and vena cava), thus decreasing flow before and after the obstruction, increasing pressure before and decreasing pressure after the obstruction (right atrium)
- squeezes the venous garden hose
- venous side flow/volume is important
- capacitance recruitment- volume how much blood pools ???
- cardiac output- pump how fast
- increased venous pressure, but decreased venous return ???
- backup at pump
- increased venous pressure increased venous return ???
- unless the increased venous return stimulates more pumping and lowers venous pressure
- looking at the pressure alone isnt enough
- resistance at vena cava (
pressure fall with flow fall
)
- as opposed to branching into capillary bed causes (
pressure fall with flow maintained
)
- IVC compression decreases uterine artery perfusion pressure and bloodflow
[NORp6]
- raises uterine venous pressure (from resistance to outlow)
- may also elevate uterine vascular resistance, decreasing flow further
- uterine venous
bloodflow decrease in pregnancy is not
significant. [NORp6]
- shunt adding to venous return
- IVC compression alone explains the diminished leg bloodflow and tachycardia with supine hypotension [NORp7]
- Uterine vein obstruction without IVC obstruction had no
change in CO or SV, but a rise in MAP in gravid ewes
- cardiac compensates for increased systemic resistance
- uterine veins higer pressure than lower systemic raise
-
IVC compression lowers Right Atrial Pressure (RAP), but hypotension does not always occur
-
Infrarenal
IVC occlusion decreases CO only
- increase HR compensates
- IVC obstruction maintains MAP by an increase HR
in gravid ewes. [NOR p6]
- kidney flow not obstructed, only lower limb so reflex vagal/sympathetic tone maintains HR
- still maintain vascualr tone thru renin from JGA
- still maintain adrenal sympathetic tone thru catecholamines
- still have renal contribution to VR
- [A?] similar to fetal occiput posterior/ late labor effect infrarenal
-
Suprarenal
IVC occlusion decreases CO & MAP ???
- lose renal contribution to VR
- lose renin and adrenal sympathetic tone ???
-
upper versus lower artery or vein effects
- venous effects seen between
contractions (without anesthesia)
- venous effects seen mostly in the supine
position (without anesthesia)
- also in lithotomy and somewhat in right lateral [NORp5]
- because veins are squishable
-
Volume pooling
(without anesthesia)
-
Supine hypotension
can occur without IVC compression [NORp6]
- from vasodilation (increased diameter of each vein)
- from increased recruitment (number) of venous vessels [?]
- labor, uteroplacental deficiency, and fetal size may increase the incidence and severity of supine hypotension.
- With
Contractions and Labor
(
no anesthesia
) [NORp7,8]
- Aortic System
- Contractions increase aortic compression and SVR [NOR p6,7]
- contracted uterus compresses aorta more than relaxed uterus [NORp7]
- compression during contractions can completely occlude the aorta [NORp7]
- mostly limited to L4-L5
- [ISLT] this effect decreases CO to offsetting the augmented VR
- The uterus displaces the infrarenal aorta laterally, cranially, and dorsally, but this is of uncertain significance. [NOR p6]
-
Aortic compression
increases MAP 10 to 20mm hg (systolic and diastolic)
- reduces CO by increased aortic compression at peak of contraction
- aortic compression effects mostly during
contractions
-
- Decreased leg bloodflow during contraction
- Dorsalis Pedis
ultrasound flow
velocities decrease 80% during contractions [NORp7]
- both in the supine and lateral
position
- see epidural effects below
- thought to be important mostly in the supine
position (without anesthesia)
- leg bloodlflow
found less in supine compared to lateral position
- some conflicting studies to this
- Painful uterine contractions may also cause aortic vasoconstriction
[NORp7]
- thru vasoconstriction due to endogenous catecholamines
- Venous System
- Uterine contractions augment CO(+25%) and SV(+30%), while lowering HR(-15%) [NORp8]
- augments Venous Return (VR)
-
uterine contraction squeezes 300ml into the central venous circulation [NORp8]
- during contractions this augments VR and offsets decreased VR from IVC compression
[NORp7]
- during
first part of contraction
- Cardiac output is a maximum 18 seconds before
maximum intrauterine pressure
- No anesthesia
/ lateral position /
Vascular Obstruction Effects
-
In the lateral positions, there is little change in cardiac parameters with contractions
-
Aortic
compression during contractions is relieved
in the lateral postition
- without regional
anesthesia
-
IVC
compression is not relieved entirely
in the lateral position by venogram (size of the vessels)
- lateral position relieves IVC compression by MRI though (flow in the vessels)
- may be reduced blood pressure rather than flow
- analogy to garden hose
- compression maintains pressure above and decreases pressure below
- decreases flow above and below
- turning faucet down
- see fig 4,5,6 p9
- Conduction blockade
[NORp334]
- Nerve block categories
-
sensory block
-
motor block
- sympathetic block
-
modulators of block duration
-
time to onset
- absorption at the site (ta)
- entry into the cell (te)
-
efectiveness of block
- potency at receptor (p)
-
duration of potency (td)
- binding constant
- time duration of effect once bound
-
clearance from the site (tc)
- important if duration of effect once bound is short compared to clearance
-
Cardiovascular effects of neuraxial blocks
[MIL,FIN]
-
Hypotension
appears to result from preganglionic sympathetic blockade
of local anesthetic agents.
- this causes both venous and arterial vasodilation, but venodilation predominates
- limited amount of smooth muscles in the venules
- large amount of blood in the venous system (approximately 75 percent of total blood volume)
- vascular smooth muscle on the arterial side of the circulation retains a considerable degree of autonomous tone
- sympathectomy and degree of hypotension that accompanies regional block is indicated by the height of sensory block
- considered two to six dermatomes above the sensory level with spinal anesthesia, and at the same level with epidural anesthesia [
MIL1496]
- however, sympathetic blockade actually extends variably above the level of sensory block
[FIN p197]
- [ISLT] may be important for ropivacaine with time-dependent pharmacodynamics
- the difficulty of predicting the degree of hypotension may relate to true variability in degrees of sympathetic block for a given sensory anesthesia level [FINp196-197]
-
venodilation increases the volume of blood in capacitance vessels and decreases VR
- this decrease in preload is the principle cause of decreased CO during high spinal
-
increased heart rate compensates for decreased stroke volumes while CO is maintained
- systolic BP>90mmHg
-
systolic BP<25% drop
- surgical patients tend to have decreased SVR
- non-surgical patients tend to have decreased CO
-
use of bupivacaine reduces the risk of hypotension
- even in the absence of clinically apparent hypotension, regional anesthesia may redistribute blood flow away from the uterus [THO p794]
- With high blockade (T1 to T4) heart rate typically decreases [MILp1496]
- direct block of the cardioaccelerator fibers
- fall in right atrial filling pressure (venous return)
- decreased outflow from intrinsic chronotropic stretch receptors
located in the right atrium and great veins
- [A?] compare to baroreceptor effects
-
Aortic and inferior vena cava compression decreases venous return [MILp2027]
- Collateral routes and increased sympathetic tone compensate for these. [MILp2027]
- Caval compression also increases uterine venous back pressure, impairing utero-placental perfusion.
- Anesthetic techniques that cause sympathetic blockade exacerbate the decreased venous return.
- a 10 degree lateral tilt will eliminate aortocaval compression in most gravidas, some only when completely on their side.
- depends on fetal position, left may be better than right lateral
- Additional injections do not significantly increase block height, but may make the block more dense (improves quality). [MILp1515]
- There appears to be a plateau affecting the dosing of epidural local aesthetics.
- When a decreased volume of local anesthetic is initially given for the epidural, and if additional local anesthetic is administered when the block height does not rise as rapidly as desired, a higher block the necessary may result, affecting arterial blood pressure. [MILp1497]
- T4 level most comfortable for C/S [MILp2049]
- Cardiac output in the supine position increases as labor progresses. [MILp2027]
- mostly from stroke volume increases and some from heart rate increase
- uterus also gets out of the way- with less compression as labor progresses.
-
Anesthesia blocks
- smaller C fibers conveying autonomic impulses are more easily blocked
than the larger sensory and motor fibers [DAVp209]
- the level of autonomic blockade extends 2-3 segments above the sensory block
- T3 blocks autonomic system completely
- implies sensory block T6-T5 blocks autonomic system completely
- "sautonomic" (sympathetic)
- "parasautonomic" (parasympathetic)
- sensory block extends above the level of motor block likewise
-
[ISLT] ropivacaine has altered ratios for nerve size effect, so cant use same criteria for assessment of sympathetic block
- sympathetic blockade
[DAVp209]
- hypotension is directly proportional to the degree of sympathetic blockade
- results in dilatation of arteries and venous capacitance vessels
- decrease in SVR systemic vascular resistance
- decrease in VR venous return
- cardiac and systemic contibutions (upper/lower)
- sympathetic block below T4
( lower splanchnic blockade )
- increased baroreceptor activity
- leads to increased reflex activity on upper cardiac sympathetic efferent fibers
- leads to reflex vasoconstriction of the upper extremities
- sympathetic block above T4
(
upper cardiac blockade )
- block of cardiac sympathetic fibers, loss of reflex
- less sympathetic to more parasympathetic ratio
for vagus
- leads to bradycardia, decreased cardiac output, and further decrease in BP
- [ISLT] depends on net combination of blocks [KAU2 p191] ???
-
neural sympathetic block (decreased lower alpha1/beta1; increased upper alpha1/beta1 from lo block)
-
neural sympathetic vagal reflex block (decreased alpha1/beta1 upper and lower from hi block)
-
humoral adrenal/ renal block (CNS beta2)
- sympathetic changes are more marked in patients who are hypovolemic
(ie, pregnant)
- viscera
[DAVp210]
- bladder
- urinary retention (T5-L1)
- increased sphincter tone from sympathetic blockade
- a catheter should be placed for prolonged anesthesia
-
intestine
- increased intestinal contraction due to parasympathetic predominance
(T5-L1)
- leads to nausea
- related to post anesthesia ileus [?]
- kidney
- 5-10% decrease in GFR and renal plasma flow, markedly decreased with hypovolemia
-
endocrine
- blocks part of the neural component of stress response
-
pain, mineralcorticoids inhibited
- inhibits adrenal (neural ) stress response through afferent sympathetic blockade to the adrenal medulla
, and pain blockade
-
abolishes the increase in blood glucose
seen during surgery
- normal glucose tolerance and insulin release maintained
- [ISLT] epidural in pregnancy would cintribute to fetal acidemia, particularly at cesarian section
-
other stress responses intact
- vagal afferent fibers from upper viscera to brain are not blocked
- can stimulate release of central ADH and ACTH (humoral )
-
motor
- motor block decreases venous return
from leg muscles [KAU2 p191]
-
thermoregulation
- vasodilation in the lower limbs leads to hypothermia
-
sensory level
- takes 20 minutes to establish
- pinprick or alcohol
-
modulators of spinal level
-
increased intraabdominal pressure
- pregnancy, obesity decrease flow within the vena cava
- this increases flow thru the epidural venous plexus,
- increases spread of local anesthetic by reducing CSF volume within the vertebral column
-
vasoconstrictors (epinephrine, phenylephrine) prolongs the duration of spinal anesthesia
-
not
with bupivacaine
-
ropivacaine
-
complications
-
hypotension
- bradycardia (sympathetic block leaves parasympathetic dominance - use atropine)
-
translocation of fluid
-
from central to the periphery as the block increases with symptoms of hypovolemia
- from peripheral to central circulation as the block recedes with hypertension (alpha1) vs tachycardia (beta1) with incresed VR ???
-
nausea and vomiting
-
hypotension and unopposed vagal stimulation (sympathetic block)
-
vagal overdischarge during transition
-
Paracervical block
[NORp264-8, 273]
-
1st stage only (no perineal anesthesia)
-
no effect on progress of labor
-
rare maternal/fetal complications
- transient
bradycardia 2-10 through 20 minutes after given
- transient fetal acidosis if lasts longer than 10 mins
- secondary to uterine artery vasoconstriction
- paracervical block has a lower incidence of fetal distress than meperidine analgesia
- maternal neuropathy 1:2000 severe buttock pain, self limited
- some perinatal deaths associated with paracervical block
- use dilute solutions for repeat blocks
- more popular in Europe than the US [THO p785]
- safe and effective
- concerns about postblock fetal bradycardia in the US
-
lidocaine 1%
-
appears in fetal blood in 5 minutes, peaks 10-20
- lidocaine increases FHR beat-to-beat variability, but no change in acid-base status
- [ANOTE] suspect that ropivacaine does this also
-
maternal lidocaine concentrations are lower for paracervical than epidural
-
2-chloroprocaine
OK but short duration
- traces only remain in fetal blood (ester)
- rapid onset and metabolism
- repeated OK
- mepivacaine
1%
- safe with and without epinephrine
- epinephrine addition may prolong delivery
-
epinephrine
prolongs duration with lidocaine or bupivacaine
- lowers maternal and fetal levels of lidocaine
- bupivacaine demonstrated to be safe (lasts about 2 hours)
- [ISLT] ropivacaine would be an appropriate anesthetic for paracervical block
-
technique
- lateral fornix of the cervix
- use needle guide
- divert the needle laterally into Frankenhauser's plexus
- wait 2 contractions for other side
- 10ml volume each side
- 4,5,7,8 oclock (4-place block has fewer failures)
-
injection into uterine arteries
- bupivacaine increases uterine tone
- lidocaine increases uterine tone less
- 2-chlorprocaine has no effect
-
fetal effects
- no real differences between bupivacaine .5%, 2-chloroprocaine 3% and mepivacaine 1% in most neonatal behavioral responses
- better pinprick response with mepivacaine at 4 hours
- [see NOR p264+]
-
Lumbar Sympathetic block
[NORp269]
-
Useful when lumbar epidural cannot be used
- Small drug volume decreases hemodynamic changes
- Afferent sympathetic nerves convey labor pain
(1st stage only), blocked by epidural
- lower uterine and cervical afferent sensory fibers enter sympathetic chain at L2 to L3
- paravertebral lumbar sympathetic block interrupts the transmission of afferent pain
impulses from the cervix and lower uterine segment at the sympathetic chain, before the nerves enter the spinal cord, also blocke by epidural
- Hypotension is common side effect
- anesthetic reaches the celiac and splanchnic plexi
- causes splanchnic vasodilation and hypotension
- Possible mechanism for decrease or increased labor due to altered sympathetic-to-parasympathetic tone with epidurals depending on level of blocks
-
Parasympathetic
efferent nerves activate longitudinal uterine muscles
-
Sympathetic
efferent nerves activate circular uterine muscles, which resist longitudinal contractions
- Lumbar sympathetic block does not interfere with the progress of labor
- uterine tone increases with lumbar sympathetic block [LEI]
-
rapid cervical dilatation accompanies lumbar sympathetic block [LEI]
- leaves parasympathetic accelerator fibers unaffected
- slow labor accompanies some epidural analgesia (other levels involved then)
- decreased uterine tone is a beta2
sympathetic effect on the uterine muscle (terbutaline)
- high lumbar epidural causes lumbar sympathetic block
- vasodilation, hypotension
- increased labor
- blocked reflex tachycardia
- [ANOTE] afferent rather than efferent
-
Epidural block
-
Epidural physiology
- the major circulatory effect of epidural local anesthetic is related to the accompanying sympathetic blockade. [NORp400]
-
causes decreased sympathetic tone
- see lumbar sympathetic block
-
mid-thoracic sympathetic blockade causes vasodilation in the lower extremities and splanchnic circulation
- reduction in venous return to the heart decreases cardiac output, which then reduces blood pressure.
- arteriolar tone (SVR) decrease plays a lesser role
- sympathetic blockade to T4 also
impairs left ventricular contractility
by inhibiting afferent cardiac sympathetic
nerve conduction (sensing for reflex)
- cardiovascular risks are low
[NORp339]
- "the major risk of unrecognized intravenous injection or infusion of dilute local anesthetic/opioids mixtures for labor epidural analgesia is inadequate pain relief, not systemic local anesthetic toxicity"
- mean heart rate increases from 85 to 90 beats per minute with ambulation
- blood pressure shows no change with ambulation
- postural hypotension is rarely a problem
-
Uterine blood flow does not decrease unless epinephrine is added or hypotension ensues. [NORp401]
-
Umbilical blood flow is unchanged.
- Adrenal
- circulating maternal plasma catecholamines
and 11-hydroxycosticosteroids are reduced with epidural anesthesia [NORp468]
- [ISLT] less maternal stress with epidural
- continuous infusions deliver more drug than an intermittent bolus injections, but amounts are still small [NORp340]
- Epidural anesthesia technique [DAV217-23]
- anesthetic acts directly on the spinal nerve roots located in the lateral part of the space
[DAVp217-23]
- anesthetic also enters the CSF thru dura
- onset of epidural block is slower
than with spinal
- intensity of the sensory and motor block is less than with spinal
-
hypotension from sympathetic blockade is similar to spinal
- large dose may lead to systemic absorption and cardiac depression
- epinephrine may be absorbed and cause tachycardia and hypertension
- [ISLT] ropivacaine has a similar effect if systemically absorbed [see ropivacaine & DAV p218]
- may increase lower limb perfusion in orthopedic surgery [218]
- reduced venous thrombosis and pulmonary embolism
-
epidural catheter should enter the epidural space midline, regardless of midline or paramedian approach [DAVp218]
- decreases the risk of puncturing epidural veins, spinal areteries, or spinal nerve roots, all of which lie in the lateral part of the epidural space
- direct placement of a needle or anesthetic into the spinal nerve may cause paresthesia [DAVp214]
- epidural veins communicate directly with the paravertebral space, and have no valves [DAVp217] ???
-
inability to thread the catheter is usually a result of the needle being inserted in the lateral part of the epidural space rather than in the midline
- bevel of the needle being at too acute an angle to the epidural space for the catheter to emerge is common
-
bevel should be pointing cephalad for catheter threading
- cautious advancement of the needle 1mm into the epidural space may facilitate catheter insertion [DAVp222]
- [see fig 16-2 p209]
-
anesthetic is injected after a test dose in 3-5 ml increments every 3-5 minutes [DAVp220]
- if injected into the CSF, spinal block neurological signs will occur
-
if injected into an epidural veins, HR will increase 20-30%
- has higher slope than spontaneous HR changes and shorter duration (30sec)
- may be blunted in pregnancy
- injection of a large volume of local anesthetic into the subarachnoid space can produce total spinal anesthesia
-
dose is reduced 30% in pregnant women
[DAVp220]
- nerves are more sensitive to local anesthetic
- inferior vena cava compression increases blood flow thru the epidural plexus, reducing the effective volume of the epidural space
- [ISLT] this would increase systemic absorption of the local anesthetic
-
modulators of epidural anesthesia
- epinephrine reduces systemic absorption
and plasma levels, prolongs duration
-
effect more marked with short acting anesthetics (lidocaine, not bupivacaine)
- fentanyl (50-100ug) shortens the onset, increases the level \, and prolongs the duration of the sensory block (see fentanyl comments)
-
neural blockade [DAVp217]
-
sensory block occurs first and is most dense at the level of injection [DAVp217]
-
block spreads faster cephalad [DAVp217]
- may be due to larger diameter lumbar and sacral nerve roots [DAVp217]
- spread is greatest at 20-30 minutes [DAVp217]
- L5-S1 is often resistant to anesthetic penetration [DAVp217]
-
sympathetic block
-
high epidural/spinal anesthesia causes preganglionic sympathetic blockade [DAVp286]
- hypotension
- bradycardia (loss of sympathetic, unopposed parasympathetic)
-
reversal of hypotension in spite of adequate volume repletion [DAVp286]
-
ephedrine 5-10mg IV
-
phenylephrine drip
- calcium chloride
in 250mg IV increments
-
[ISLT] factors that acutely lower calcium concentration predispose to hypotension
-
low estrogen (PTL, IUGR)
- low dietary calcium (Teens, Eating disorders, Nutritional defieciencies)
- dyspneic sensation may be experienced with higher spinal block (block of afferent sensation fibers) [DAVp216]
- Uterine activity / course of labor
[NORp345-414, THO]
- uterine innervation
-
Parasympathetic
efferent nerves activate longitudinal uterine muscles
-
Sympathetic
efferent nerves activate circular uterine muscles that resist longitudinal contractions
- see epidural block
-
modulators
- intravenous fluids associated with conduction of epidural analgesia can transiently decrease uterine activity [NORp345]
- [ISLT] decreased oxytocin (neural)
-
supine position results in more frequent, less intense uterine contractions with increased basal uterine tone.
- [ISLT] higher sympathetic tone in supine position
- lateral position results in less frequent, more effective uterine contractions
- [ISLT] less sympathetic tone in lateral position
-
better blood flow to uterus in between contractions
- drug effects on labor [THO]
- lower concentration of the epidural anesthetic has lower adverse risk
- More concentrated local anesthetic solutions may increase the risk of operative delivery. [NORp351]
- thought due to more motor block
- [A?] may be less uterine contractions from sympathetic block[?]
-
bupivacaine has a higher rate of cesarian section than for lidocaine
- addition of fentanyl to bupivacaine for epidural increases the cesarian section rate 7x
[p788 THO]
- combined spinal(intrathecal)-epidural with sufentanyl prolongs labor
compared to IV narcotics
-
intrathecal sufentanyl
increases the risk of fetal bradycardia necessitating emergency cesarian section
- unclear whether this was from reduced uteroplacental blood flow or hyperstimulation
- [A?] effects of block on hyperstimulation
-
few randomized prospective trials
have examined the impact of epidural analgesia on the risk of cesarean delivery for dystocia. [NORp357 1999]
-
level I studies (at least one properly designed randomized study [THO]
-
epidural can prolong labor, but
- slows cervical dilatation
- prolongs the active phase of labor
- prolongs the second stage of labor
- see lumbar sympathetic block however
-
epidural causes increased requirement for oxytocin augmentation
- more oxtocin required to achieve the same cervical change
-
epidural increases requirement for instrumental delivery
-
conflicting evidence that epidural anesthesia increases cesarian section rates
- studies with better compliance and less crossover showed increased rate
- cesarian birth rate for non-reassuring fetal heart rate tracing increased with epidural and spinal anesthesia
- [ANOTE] may require more patience to allow porgress of labor
-
1st stage
- the effects of epidural analgesia on 1st stage are inconsistent
- in retrospective studies, women who requested epidural analgesia already had signs of abnormal labor before they received any anesthetic intervention
- Patients receive epidural labor analgesia at less cervical dilation reference point. Patients receive epidural labor analgesia at less cervical dilation reference point.
- epidural labor analgesia before 5 cm cervical dilation does not
increase the risk of dystocia [NORp359]
-
2nd stage
-
Epidural anesthesia appears to prolong the second stage
of labor in prospective randomized studies.
-
no increase in the duration of labor or the use of forceps for delivery if continue a dilute bupivacaine/fentanyl infusion compared with saline and better pain relief in the second stage [NORp353]
-
effects on labor may be related to (para)sympathetic blockade to the uterus
- partially blocking pelvic parasympathetic efferent outflow (contractions) with epidural analgesia may slow labor,
without affecting
sympathetic
efferents (tocolysis) [see LEI p1044 fig] ???
- low level epidural block has increased sympathetic
tone, decreased parasympathtic
tone to the uterus, which slows labor (no lumbar sympathetic block)
- hi level epidural block has decreased
sympathetic tone to the uterus, which speeds labor
-
see lumbar sympathetic block
- unclear whether the timing of epidural and active management affect labor with epidurals [THO]
-
station at the time of epidural administration is a better predictor of cesarian risk than cervical dilatation
- delayed pushing allows more spontaneous vaginal deliveries and fewer forceps deliveries without any fetal compromise [NORp355]
- obstetricians with lower rate of cesarean section intervened earlier in the second stage with forceps or vacuum [NORp346-51]
-
Epidural effects in pregnancy
- Considerations for epidural
[NORp406]
- mother is most comfortable when block exceeds T5 level
-
pt experienced pain only if if block below T5 (2 dermatomes below the level of analgesia by loss of sharp pin-prick for lidocaine)
- exteriorizing uterus at C/S requires more extensive block
- local anesthetic concentrations may be higher in acidotic infants
- basic compounds (local anesthetics) trapped within the placenta and the fetus as the charged form
- hydrophilic water soluble compounds (less lipophilic like morphine, ropivacaine) more trapped than bupivacaine, less than lidocaine
-
lidocaine better with fetal distress
- opioids allow the use of more dilute local anesthetics by potentiating the effects of local anesthetics. [NORp631]
- Lumbar epidural may improve uteroplacental perfusion by reducing maternal circulating catecholamines with bupivicaine (relieve stress from pain), with improvement of intervillous blood flow in preeclamptic patients. [NORp630]
-
Vascular effects
- peripheral vasodilation and venous pooling [NOR p7]
- secondary to the loss of sympathetic tone (alpha1) from epidural
- decreases venous return (less alpha1)
- decreased splanchinc return (less alpha1)
- causes decreased MAP (less alpha1)
- [A?] does epidural augment peripheral blood flow at the expense of central blood flow
- compromises the ability to compensate for a fall in venous return [NORp6]
- cardiac output and uterine artery perfusion depend on adequate venous return
- femoral artery (leg) hypotension occurs earlier and more commonly than brachial artery (arm) hypotension with regional anesthesia.
- systolic pressure decreases more than diastolic in the femoral artery with aortic compression. [see NOR p7 figure out] [???]
- decreased pulse pressure in the femoral artery
-
leg MAP found not to change with position
- Aortic compression does not cause decreased leg bloodflow in the presence of normal leg MAP
- lumbar epidural anesthesia improves the dorsalis pedis flow velocities which are normally decreased in laboring women
in supine or lateral positions [NORp7]
-
[A?] redistribution of blood flow into extremities
-
Hypovolemia/ hypotension cardiovascular epidural effects
-
decreases venous return
-
hypotension and fetal acedemia
- regional anesthesia may result in redistribution of cardiac output away from the uteroplacental unit, as well as produce systemic hypotension, resulting in umbilical cord acidemia [THOp798]
- "The potential for regional analgesia/anesthesia to cause significant decompensation in uteroplacental function ...is well documented." [THOp795]
-
5-fold increased risk for spinal, 2-fold increase for epidural anesthesia
- primarily respiratory in origin [A?] maternal hypoventilation
- level I studies (at least one properly designed randomized study) [THO]
- epidural analgesia
-
lower umbilical arterial pH
-
higher arterial pCO2
- higher arterial bicarbonate values
- indicates a fetal acidemia
-
Perineal trauma
- epidural analgesia increases the occurence of severe perineal trauma
- level II studies (non-random or retrospective study) [THO]
-
Maternal fever
- evidence that epidural increases incidence of maternal fever. The mechanism is unclear.
- level I [THO]
-
Intrathecal Block
-
Spinal Block
- Spinal anesthesia hemodynamics
[NORp418]
-
hypotension develops less often in laboring women
- hypotension develops in proportion to the extent the sympathetic blockade
[NORp419]
- increases venous capacitance
- decreases arteriolar tone
- decreases cardiac output
- diastolic pressure can decrease more than systolic pressure (
increases pulse pressure, decreases MAP
). [NORp419]
-
sensory blockade above T5
cause more significant hypotension through a block of cardiac sympathetic nerves.
- in this setting, compensatory tachycardia does not accompany decreases in blood pressure. heart rate decreases as blood pressure decreases.
- in other settings, hypotension is accompanied by compensatory tachycardia
- Control of venous capacitance lies in the mesenteric venous system, not in the leg veins.
-
mesenteric venodilation from sympathetic blockade of the splanchnic circulation is the most important cause of this increased venous capacitance.
-
decreases
central venous pressure (CVP)
and left ventricular end diastolic volume (LEDV)
- reduces cardiac output, stroke volume, and therefore blood pressure [NORp419]
- Maternal hemodynamic changes with spinal anesthestia can affect the fetus
- maternal systolic hypotension below 70mmHg correlated with the incidence of fetal bradycardia
in severity and duration (see blood pressure measurement issues)
- uterine artery pulsatility index shows no consistent changes with spinal anesthesia
- The changes seen did not correlate with any hemodynamic event, Apgar or umbilical artery scores. [NORp420]
- increases in the pulsatility index reflect vasoconstriction
- inconsistencies because of cardiac vs splanchnic vs lower
venous sympathetic variability
- The effects of transient maternal hypotension are less clear.
- prolonged time to sustained respirations has been reported
.
- Even when treated with ephedrine, infants born of mothers with periods of maternal hypotension (systolic blood pressure <100mmHg or a decrease of more than 30 from baseline) of less than 3 minutes showed slightly lower umbilical artery pH, although still within normal limits. [NORp422]
- Neurobehavioral studies were normal. [NORp422]
- Other studies when ephedrine was used indicate no differences. [NORp422]
-
Volume loading:
- increases maternal CVP and ameliorates the hypotension with spinal anesthesia for C/S. [NORp423]
- releases atrial natriuretic peptide (ANP), causing vasodilation and naturesis. [NORp424]
- may diminish the fetal effects of maternal hypotension caused by spinal anesthesia, such as the incidence of fetal acedemia (pH <7.2). current studies have not been sufficient to answer this question. [NORp424]
- with fluid preloading using ephedrine infusion to maintain blood pressure for spinal anesthesia, there was an increase in the umbilical artery pulsatility index at 30 minutes (but not at 15) by pulsed doppler measurements (indicating decreased diastolic blood flow at 30 mins). [NORp420]
- Head-down tilt (Trendelenberg) has little or no effect on the blood pressure changes with spinal anesthesia
[NORp423]
- needle should enter epidural space midline, as space is widest there and decreased risk of puncturing epidural veins
-
Fentanyl 6.25mcg added to spinal anesthesia improves post operative pain.
- More than 15mcg increases the incidence of itching, with significant maternal sedation and hypotension.
[NORp432]
-
Maternal Complications of Regional Anesthesia
-
Hypotension
- Hypotension is the most common complication of obstetric regional anesthesia
[NORp593]
- Mild hypotension produces few maternal symptoms but is poorly tolerated by the fetus.
- Neuraxial blocks are similar
in some ways to the combined use of intravenous alpha1 and beta adrenergic blockers
[MIL2031-39]
- Uterine blood flow falls in proportion to the decrease in maternal blood pressure
- UBF not related to maternal heart rate, because a low pressure system
- Infants of hypotensive mothers (mean arterial pressure less than 70 mm Hg during epidural anesthesia for cesarian section) had normal Apgar scores but weak rooting and suckling reflexes for 2 days
in one study, . [NOR p593, 614 ref 8]
- fetal effects delayed with regional anesthesia [?]
- IV prehydration fails to reliably prevent hypotension and lowers maternal colloidal osmotic pressure. [NORp596]
- Systemic hypotension stimulates baroreceptors and may increase heart rate [NORp612]
- The vasodilational effects of lower level sympathetic block is modified by a compensatory increase in sympathetic tone and vasoconstriction in unblocked areas, resulting essentially in very little change in SVR. High-level block or concomitant general anesthesia increases the likelihood for hypotension by nullifying the ability to compensate.
- When CO and SVR both decrease during spinal
anesthesia, the SVR reduction preceeds
the CO reduction. [FINp196] ???
-
Hypovolemia during regional anesthesia
- spinal and epidural anesthesia induce a form of distributive hypovolemia, when the cardiac preload decreases (but not afterload) [NORp594]
- CVP falls
in all patients with spinal anesthesia
- Stroke volume and End-diastolic volume diminish during hypotension, while SVR barely changes. [NORp595]
- Ephedrine or phenylephrine treatment restores BP, SV, EDV to baseline values, while decreasing SVR. ??? [NORp595, see fig2]
- see Ephedrine
-
Tachycardia
- Healthy pregnant women are relatively insensitive to chronotropic agents. [NOR p602]
-
Increasing the heart rate 25 BPM
requires five times as much isoproteronol in healthy pregnant women as in nonpregnant women
. [NORp602]
- maternal heart rate can increase more than 30 BPM with each painful uterine contraction in 12-45% of laboring women [NORp602]
-
Some laboring women never become tachycardic, and actually experience bradycardia. [NOR p602]
- Epinephrine, a mixed alpha and beta agonist, does not consistently produce maternal tachycardia.
[NORp602, fig 4,5] [NORp596]
- Occasionally ephedrine has predominantly beta-adrenergic effects. [NORp602, fig 4,5] [NORp596] ???
- Arterial hypotension obtained with direct vasodilating drugs and with calcium channel blocker nicardipine frequently incurs reflex tachycardia. [MILp1142] ???nifedipine/pregnant
- Hypercarbia
-
All causes of increased oxygen consumption also increase carbon dioxide production [MILp611]
- Hypoxia causes based deficit and increased lactate to pyruvate ratio (acidosis) [MILp611]
- Treatment with Pressors/ Ephedrine
[NORp596-7]
- Small amounts of a venoconstrictor
to a hydrated, laterally tilted patient can restore cardiac preload without affecting uterine blood flow.
- Ephedrine does not decrease uterine blood flow in unanesthetized ewes despite a 50% increase in maternal blood pressure.
-
Ephedrine is the pressor of choice
during obstetric anesthesia. No theraputic agent surpasses its performance. [MILp2031]
- Both animal data and years of clinical use support its beneficial effects of increasing maternal blood pressure, cardiac output, uterine blood flow, and fetal status when used to treat hypotension.
- Uterine blood flow was not adversely affected by doses of ephedrine which increased maternal blood pressure up to 50 percent in pregnant sheep.
- Prompt treatment of hypotension with ephedrine restores maternal blood pressure and cardiac output. The goal is to maintain cardiac preload.
- Ephedrine restores uterine blood flow to 90% of baseline
value in gravid ewes with spinal-induced hypotension.
- Ephedrine elevates maternal heart rate if depressed (chronotropy) and cardiac contactility (inotropy).
- prophylactic IM treatment does not prevent maternal hypotension [NORp425-6]
- Ephedrine with spinal anesthesia [NORp425-6]
- Datta et al recommend giving 10 to 30 mg of IV ephedrine "as soon as any fall from baseline pressure" occurs. [ref 93, p425,438]
- Neonates in this group had better acid-base and Apgar parameters than those who received it only after blood pressure had dropped by more than 30 mm Hg
or to less than 100 mm Hg.
-
Ephedrine crosses the placenta, and can cause fetal tachycardia, release of fetal catacholamines, and (transiently) decrease neonatal EEG delta wave activity.
- This was a sequential, non-randomized study, and may have been complicated by infusion of dextrose. The need to use ephedrine to insure a good outcome remains unclear.
- a vasopressor is often required because fluids alone are ineffective at preventing or correcting maternal hypotension from sympathetic blockade [NORp626]
- the vasopressor of choice is ephedrine
- Its beta-adrenergic effects increase maternal heart rate, contractility, cardiac output and uterine blood flow.
- the reflex parasympathetic effects and decreased chronotropic sensitivity to sympathetic stimulants in laboring patients
would make ephedrine more appropriate in this setting as noted
- [ISLT] since ropivacaine is less cardio-depressant than bupivacaine, might expect more reflex tachycardia from epidural hypotension with ropivacaine than with bupivacaine
- [A?]also since time dependant, ropivacaine would have delayed effects relative to other anesthetics
-
Ephedrine crosses the placenta, increases fetal heart rate and beat-to-beat variability.
-
Phenylephrine, a pure alpha agonist can be used instead of ephedrine to maintain blood pressure after regional blockade.
- Phenylephrine also restores maternal BP and cardiac preload while ensuring good neonatal acid-base status, Apgar scores and neurobehavioral scores. [NOR]
- In non-laboring
patients it has been shown as effective as ephedrine, without adverse neonatal effects.
- Phenylephrine is often used in the setting of tachycardia secondary to beta agonist, when the maternal heart rate is over 100BPM. [NORp643]
- effects of phenylephrine on the compromised fetus have not been studied
[see NOR p626].
- Sympathetics/parasympathetics affect the progress of labor [LEIp1044]
-
lumbar sympathetics inhibit labor
- alpha2 sympathetic central tone increase inhibits uterine contractions (NE)
- fright
- higher than T3 level
- low-dose lumbar epidural would not affect these sympathetic efferents
- beta2 sympathetic receptors in uterus decrease uterine tone (beta2)
- epinephrine
inhibits uterine tone at term [p150G&G]
- terbutaline
- beta blocker speeds labor (propanolol)
-
pelvic and sacral parasympathetics speed labor
- increase uterine contractions
- block delays the onset and increases duration of labor
-
slow labor
accompanies low epidural
analgesia
-
fast labor
accompanies lumbar sympathetic block
- sympathetic nerve block develops more quickly in pregnant women during regional anesthesia [NOR p594]
- possible mechanism for decrease or increased labor due to a reflex increased sympathetic-to-parasympathetic tone with epidurals
- rapid cervical dilatation accompanies lumbar sympathetic blockade. [LEI]
- leaves accelerator parasympathetic fibers unaffected, speeds labor
- plasma epinephrine level is not the cause of this
- lumbar epidural, lumbar sympathetic block both decrease plasma epinephrine
-
Obstetric issues
-
recommend giving epidural when primip dilation is 5-6cm, multip dilation 3-4cm
-
spinal saddle block gives motor blockade
- forceps
- laceration repair
-
An anesthesiologist talks analgesia choices
Anna Nidecker, OBGYN News Nov1, 1996, p21
meeting on obstetrics and obstetric anesthesia by St. John Hospital and Medical Center in Detroit
Dr. Callum R. Hoyt, chief of obstetric anesthesiology at Case Western Reserve
- Dr. Hoyt condemned the practice of stopping the epidural in the second stage of labor.
[p21]
- patchy, one-sided or failed epidurals produce more painful labor
than if the woman had not received an epidural in the first place.
-
0.125% bupivacaine
recommended
- "paracervical blocks are making a comeback", says Dr. Hoyt
-
nitroglycerin relaxes the uterus
-
nitroglycerin for the entraped head with breech delivery, retained placenta, and inverted uterus, rather than general anesthesia is a possibility, with less risk.
-
"quick administration of a spinal does not reduce maternal blood flow to the fetus to the extent that general anesthesia does."
-
Fetal status
- The intrapartum fetal heart rate tracing is the only monitor of intrapartum fetal status.
- Beat to beat variability of the fetal heart rate is the most important parameter in predicting fetal hypoxemia. Beat to beat variability represents the constant push-pull effect of the sympathetic and parasympathetic nervous systems on the fetal heart, and indicates an intact axis between the central nervous and cardiovascular systems. [NORp620]
- Loss of beat-to-beat or short term variability, combined with late decelerations, raises serious concerns about fetal well being (hypoxemia). [NORp632]
- Persistent, irreversible loss of beat to beat variability, devoid of accelerations or decelerations in the fetal heart rate tracing, should alert the clinician to the development of true fetal distress. [NORp623-4]
- [ANOTE] contradictory- hypoxemia vs acidemia
- Loss of baseline (???longterm) variability correlates well with umbilical artery acidemia
at birth
-
Decelerations
-
Fetal heart rate decelerations are mediated by chemoreceptor (hi pCO2, low O2) and baroreceptor (low BP) stimulation of the fetal vagus nerve. [NORp622]
-
IV analgesics interfere with fetal heart rate analysis.
- Epidural opioids, like systemic opioids, may affect fetal heart rate patterns and neonatal status. [NORp631]
- Epidural fentanyl does not cause neonatal depression as measured by Apgar scores and respiratory rates after delivery when there is no fetal compromise. [NORp632]
- IV injection of 50 to 75 mcg of fentanyl has no significant impact on fetal heart rate patterns. ???
-
Hypotension
- aggressive treatment with ephedrine and additional IV fluids, produces no differences between infants born to mothers who developed hypotension and those who remained normotensive. [NORp408]
- Except in those unusual circumstances where maternal blood pressure is known to be excessive (as in severe preeclampsia), empirically increasing maternal blood pressure in the face of fetal compromise is indicated. [PALp26]
-
significant maternal hypotension may risk both umbilical acidosis and depressed neurobehavioral scores
-
"Infants whose mothers experienced 4-8 minutes of hypotension during the induction of epidural anesthesia for cesarian section had abnormal neurobehavioral tests for 2 days." [NORp417]
-
Hypoxemia
- Anaerobic glycolysis in underperfused, vascular beds produces a metabolic acidosis
, which is completely reversible if fetal hypoxemia is corrected within one hour. [NORp620]
-
fetal vs maternal
- [A?] fetal hypoxemia produces metabolic (lactic) acidosis (high fetal oxygen demand), but low placental blood flow can allow an accumulation of CO2 which produces respiratory (CO2) acidosis (normal fetal oxygen demand)
-
Asphyxia
-
Fetal deterioration usually follows a continuum as a chronically compromised or stressed fetus is further deprived of nutritional blood flow and becomes hypoxemic and distressed. This can be likened to the development of myocardial ischemia before myocardial infarction. [NORp620]
-
The intact fetus develops tachycardia in an attempt to increase cardiac output and oxygen delivery in response to asphyxia.
-
Aspyxia involves hypoxemia, hypercapnia, and fetal circulatory insufficiency
.
-
Later systemic vascular resistance in reflex bradycardia or decelerations of the fetal heart rate occur [NORp622] ???
- dont like the term asphyxia since imprecise
-
lower oxygen concentration that is ok for aerobic metabolism
-
is there a cutoff value for oxygen tension
-
role of fetal acidosis
-
Fetal outcomes
[NORp620]
-
Fetal Acidemia
[MUE]
- more Fetal Acidemia after regional anesthesia for elective cesarian delivery [MUE]
- fetal acidemia (pH less than 7.10) was significantly increased with spinal anesthesia
and in the epidural group
(odds ratio 4.67 and 2.39) compared with general anesthesia
- in non-laboring patients, spinal anesthesia will be followed by hypotension
despite prophylaxsis.
-
Apgar scores at 5 minutes were consistently higher after regional anesthesia than general
-
[ISLT] may indicate immediate fetal advantage
- may indicate a sleepy newborn or less newborn stress from general anesthesia, rather than a fetal depression
- may indicate fetal hypoperfusion
- may indicate maternal hypoperfusion
- Fetal stress
[NORp391-2]
-
Cord (fetal) epinephrine concentrations are higher after epidural
than with general anesthesia, but mother epinephrine plasma levels are lower.
- [A?] baby has stress, not mom with epidural
- there are no immediate
differences in neonatal beta-endorphin concentrations in babies born after epidural anesthesia compared to general anesthesia.
- at 2 hours, when epinephrine drops, infant has higher beta-endorphin levels with epidural
- The risk of low cord pH was 4.7 times higher for spinal and 2.4 times higher for epidural anesthesia
than for general anesthesia.
- [A?] suspect secondary to less maternal hyperventilation
- Anesthetic technique does not correlate with neonatal mortality.
- No correlation is found between neonatal outcome and induction to delivery interval
- no differences in neurobehavioral scores when delivered by C/S between epidural lidocaine, bupivacaine, 2-chloroprocaine, or ropivacaine. [NORp410]
- [ISLT] Few studies have compared nenatal outcomes between regional and general anesthesia for emergency cesarian section (because of time course may not see epidural late cardiovascular effects at emergency C/S) [NORp633]
-
Thermoregulation and anesthesia [SES]
- obese people are more vasodilated at onset of anesthesia
-
heat loss
-
radiation ~10% heat loss
-
respiratory can be ~10% heat loss
-
get redistribution of heat to periphery, not net loss with regional(1/2) and general anesthesia ???
- general, central, regional, peripheral
- core temperature drops
- alpha3 to brown fat heat loss ~10% in hypothermia
-
reduction in metabolism
- alpha1, augmented by local alpha 2, gives vasoconstriction of AV shunt
-
opioids and propofol linearly decrease the vasoconstriction and shivering thresholds
-
Anesthesia Services
- Anesthesia is the sixth leading cause of pregnancy-associated maternal mortality. [ref 19 see NORp 769,778]
- inhalation anesthesia is the largest part
-
Standards for conduction anesthesia
[sp473]
-
Standard I
-
appropriate resuscitation equipment must be available
-
Standard II
-
major conduction blocks in obstetrics shall be initiated and maintained by or under the direction of a physician with appropriate privileges
-
physicians must be approved to administer or supervise the obstetric anesthesia, and must be qualified to manage to procedurally related complications
-
Standard III
-
major conduction anesthesia should not be administered until the patient has been examined and the fetal status and progress of labor evaluated by a qualified physician who is readily available to supervise and deal with any obstetric complications that may arise.
-
standards may be exceeded based on the judgement of the responsible anesthesiologist
- [ANOTE] these standards have been relaxed
-
Ethics [NORp769]
- the study of the general nature of morals and of the specific moral choices to be made by a person.
- the rules
governing the conduct of a person or members and standards
of a profession (group).
- [ANOTE] we need to clarify the duties and responsibilities of individuals versus groups
Back
 page views since Jan2005
page views since Jan2005