|
Clinical Benefits of Estrogen (Easy Part)
- Bone, Joints and Skin
- Osteoporosis, which imobilizes more women than any other disease in
advanced old age, is entirely prevented with Estrogen treatment. Estrogen
makes bones strong, improving Calcium content and Vitamin D levels.
Estrogen inhibits Osteoarthritis. 1
- Bone and Joint pain is associated with Estrogen deficiency, and reversed with
Estrogen therapy. 2
- Skin looks younger and softer with Estrogen 3
- 30-50% of skin collagen depends on Estrogen, which prevents and
repairs damaged skin. 3a
- Small blood vessels that nourish the skin, vaginal skin health and
lubrication, requires Estrogen
- Low Estrogen impairs wound healing 4
- Brain Function and Sleep
- Improves sleep and integration of brain activity 12
- Improves memory 6 , inhibits Alzheimers onset 7
- Improves coordination 8
- Improves mood, stabilizes lability (loss of control, emotions) 8
- Heart & Vascular Disease
- Inhibits arterial plaques (arterial disease) caused by low Estrogen 10
- Maintains smooth muscle function of blood vessels (better blood flow and
tissue perfusion) 11
- Lowers total Cholesterol, increases HDL 12
- Lowers Heart Disease and Mortality when started near menopause 13
- Mortality
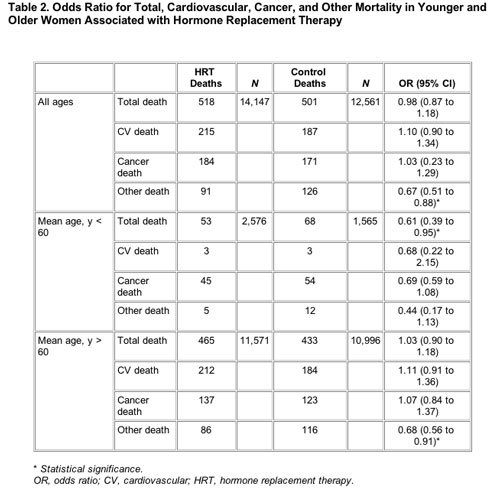
- Observational Studies (retrospective and prospective) indicate the same or lower
mortality with Estrogen and Estrogen/Progestin therapy. WHI does not contradict these findings, (and in fact a further analysis of WHI now shows a decreased mortality of 30% between 50-60 years of age with either Estrogen or Estrogen+Progestin).(c) 14
- Estrogen benefit for Mortality from Cardiac Disease is highly dependent on the
severity of disease 15
- Estrogen treatment decreases mortality after Breast Cancer(a) 16,49
- Cancer
- Overweight women have a higher risk of breast cancer (the major risk factor) 17
- Apoptosis (programmed cell disintegration) plays an important role in
preventing cancer, is modulated by steroid hormones 18
- Breast cancer risk is associated with an increase in Free Estradiol produced from the Tumor, not causing the Tumor (as with Menopausal transition, Obesity or Anovulation)(b) 19
- Breast cancer cell lines resistant to Estrogen deprivation undergo cell death
when treated with menopausal concentrations of estradiol. The Estrogen is
100% effective in killing the cancer cells. 46
- Hot Flashes
- Currently the least controversial benefit for Estrogen is treatment of hot flashes 20
- Sex Drive
- Libido and energy depend on Free Testosterone (converted from Estradiol) 21,51
- Obesity
- Estrogen reduces tummy fat at menopause 22
- Estrogen lowers blood sugar and prevents onset of diabetes 24
- Immune System
- Estrogen improves Immune function and Rheumatoid Arthritis 25
- Thrombosis concern note
- Hemorrhagic Stroke (caused by bleeding, more severe, 10% of strokes) is
reduced by Estrogen, but Thrombotic Stroke (ischemia caused by clotting,
less severe, 90% of strokes) may be increased by Estrogen (the evidence is
conflicting). 26
This is mostly seen in the first year of use and for older women, with indications
of no increase for total stroke in the younger age group 50-59. Stroke mortality
is not affected in any age group.
- Estrogen actually increases the rate of clot lysis. 27
- Estrogen keeps brain tissue healthier, but may adversely affect brain tissue
that is already damaged. Neural blood vessels 8 and nerve growth 6
are adversely affected by a lack of Estrogen.
- Thrombotic risks may be related to increased levels of Free rather than
Total Estrogen, and not in a simple way.
- Statins, Aspirin (COX-1) and certain tNSAIDS ("traditional" less COX selective) alter
cardiovascular risk and the effect of estrogen. They appear to lower Thrombotic
Stroke and Heart Attack rates, preventing initial adverse effects of hormone
supplements in older, high-risk women. 30 Discontinuing Aspirin or NSAIDS,
in contrast increases Stroke and MI. 48
- Age and vascular disease severity appears to increase the risk of Thrombotic
Stroke and MI, and effects of estrogen and NSAIDS.
|
|